Complications
Cor pulmonale is right-sided heart failure secondary to longstanding COPD. It is caused by chronic hypoxia and subsequent vasoconstriction in pulmonary vasculature that causes pulmonary hypertension and right-sided heart failure.
Engorged neck veins, a loud P2, lower-extremity edema, and hepatomegaly are signs of cor pulmonale.
Continuous oxygen therapy is the mainstay of therapy. Therapy for COPD should be optimised. Judicious use of diuretics is warranted.[269]
COPD is a risk factor for lung cancer independently of tobacco exposure. A population-based cohort study found that, compared with never-smokers without COPD, the fully-adjusted hazard ratios for lung cancer in never-smokers with COPD, ever-smokers without COPD, and ever-smokers with COPD were 2.67, 1.97, and 6.19, respectively.[273]
Recurrent pneumonia is a common complication of COPD and a frequent cause of COPD exacerbation. Either viral or bacterial infections can be the cause.
Chronic lung and airway damage, inflammation, compromised ciliary function, and bacterial colonization are likely causes of increased vulnerability to infections. Use of inhaled corticosteroids is also associated with increased risk of pneumonia in patients with COPD.[124][266][267]
Use of antibiotic therapy has shown some benefit.[268] Usual treatment time is around 7-14 days. Appropriate coverage for Haemophilus influenzae and Streptococcus pneumoniae is mandatory. Pneumococcal vaccination is strongly recommended in patients with COPD.
Depression is a common consequence of COPD. It is estimated that patients with COPD are 1.9 times more likely to die from suicide than those without COPD.[157] If any mood change occurs, a psychiatric evaluation may be necessary.
Occurs because of lung parenchyma damage with subpleural bulla formation and rupture. Spontaneous pneumothorax is very common with chronic severe cough or chest trauma, and may be life-threatening.
High levels of suspicion are necessary for prompt diagnosis. Chest x-ray or chest computed tomography (CT) confirms the diagnosis.[Figure caption and citation for the preceding image starts]: Chest CT: severe COPD changes with right pneumothoraxFrom the collection of Manoochehr Abadian Sharifabad, MD [Citation ends].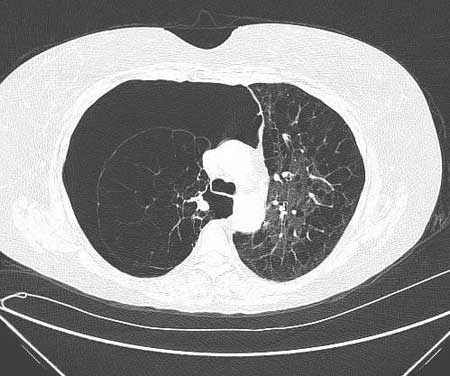
Conservative management may be sufficient in minor cases. In severe cases, chest tube insertion is necessary to prevent tension pneumothorax and hemodynamic instability. If recurrent pneumothorax occurs, then surgical interventions, such as video-assisted thoracoscopy pleurodesis or bullectomy, are warranted.
A study of a large number of patients with COPD and acute respiratory failure reported in-hospital mortality of 17% to 49%.[265] Therapy includes noninvasive positive pressure ventilation and/or mechanical ventilation.
Anemia is more prevalent than previously thought, affecting almost 25% of patients with COPD.[270] A low hematocrit indicates a poor prognosis in patients receiving long-term oxygen treatment.[271] One meta-analysis found that patients with comorbid anemia were also more likely to spend longer periods of time in the hospital than those without comorbid anemia, as well as experiencing higher rates of mortality.[272]
Secondary polycythemia can develop in the presence of arterial hypoxemia, especially in continuing smokers. It can be identified by hematocrit >55%. Many times these patients require supplemental home oxygen.
Use of this content is subject to our disclaimer
