Investigações
Primeiras investigações a serem solicitadas
spirometry
Exame
Test establishes FEV₁ and FVC. The ratio of these two values indicates whether airflow obstruction is present. COPD severity is classified based on the patient's FEV₁ and its percentage of the predicted FEV₁. In cases where FVC may be hard to measure, FEV₆ (forced expiratory volume at 6 seconds) can be used.[67]
Spirometry should be performed after administering an adequate dose of at least one short-acting inhaled bronchodilator to minimize variability.[1]
A primary care doctor explains how to perform spirometry and how to avoid any pitfalls.
A guide on how to perform and interpret spirometry, including common pitfalls.
Resultado
FEV₁/FVC ratio <0.7; total absence of reversibility is neither required nor the most typical result
standardized symptoms score
Exame
In addition to airflow limitation, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recognize the importance of exacerbations in affecting the natural course of COPD, and place emphasis on assessment of symptoms, risk factors for exacerbations, and comorbidities.[1]
The Modified British Medical Research Council (mMRC) questionnaire or the COPD Assessment Test (CAT) are recommended to assess symptoms. GOLD cautions against the use of the mMRC dyspnea scale alone for assessing patients, as symptoms of COPD go beyond dyspnea alone. For this reason, the CAT is preferred. However, GOLD acknowledges that the use of the mMRC scale is widespread, and so a threshold of an mMRC grade ≥2 is still included to define "more breathless" patients, as opposed to "less breathless" patients, in its assessment criteria.[1]
Resultado
mMRC score ranges from 0-4; CAT score ranges from 0-40: mMRC ≥2 or CAT score ≥10 indicates higher symptoms burden
pulse oximetry
Exame
Checked as part of vital signs on acute presentation. A good pulse wave should be picked up by the device. In patients with chronic disease, an oxygen saturation of 88% to 90% may be acceptable.
If ≤92%, arterial blood gases (ABG) should be checked.[1]
Resultado
low oxygen saturation
ABG
Exame
Checked in patients who are acutely sick, especially if they have an abnormal pulse oximetry reading. Should also be performed in stable patients with FEV₁ <35% predicted or with clinical signs suggestive of respiratory failure, or if peripheral arterial oxygen saturation is ≤92%.
Hypercapnia, hypoxia, and respiratory acidosis are signs of impending respiratory failure and possible need for intubation.
Resultado
PaCO₂ >50 mmHg and/or PaO₂ of <60 mmHg suggests respiratory insufficiency
Chest x-ray
Exame
Seldom diagnostic, but useful in ruling out other pathologies and in assessing for the presence of significant comorbidities (e.g., pulmonary fibrosis, cardiomegaly).[1]
Increased anteroposterior ratio, flattened diaphragm, increased intercostal spaces, and hyperlucent lungs may be seen. [Figure caption and citation for the preceding image starts]: COPD chest x-ray (AP view): hyperinflated lung, flattened diaphragm, increased intercostal spacesFrom the collection of Manoochehr Abadian Sharifabad, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: COPD chest x-ray (lateral view): hyperinflated lung, flattened diaphragm, increased antero-posterior diameter (barrel chest) in lateral viewFrom the collection of Manoochehr Abadian Sharifabad, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: COPD chest x-ray (lateral view): hyperinflated lung, flattened diaphragm, increased antero-posterior diameter (barrel chest) in lateral viewFrom the collection of Manoochehr Abadian Sharifabad, MD [Citation ends].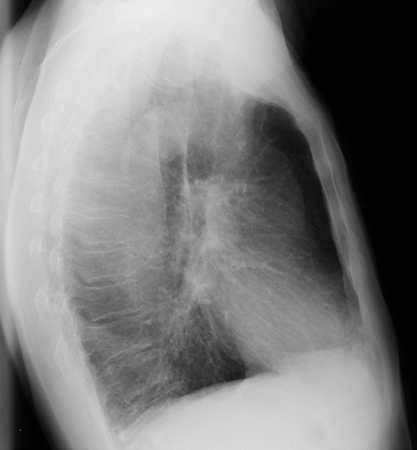
May also demonstrate complications of COPD, such as pneumonia and pneumothorax.
Resultado
hyperinflation
CBC
Exame
This test may be considered to assess severity of an exacerbation and may show polycythemia (hematocrit >55%), anemia, and leukocytosis. UK guidelines advise CBC in all newly diagnosed patients.[2]
Resultado
elevated hematocrit, anemia, possible increased WBC count
Investigações a serem consideradas
pulmonary function tests
Exame
Detailed pulmonary function tests performed in specialist pulmonary function laboratories can measure flow volume loops and inspiratory capacity. They are not used routinely but can be helpful in resolving diagnostic uncertainties and for preoperative assessment.
Diffusing capacity of the lung for carbon monoxide (DLCO) was previously only measured in specialist laboratories; however, portable systems are now available, allowing measurements to be taken in the field. International guidelines from GOLD recommend a DLCO measurement if a patient with COPD has dyspnea that is disproportionate to their degree of airflow obstruction. A low DLCO value (<60% predicted) in a patient with COPD is associated with decreased exercise capacity, worse health status, and increased risk of death.[1]
结果
obstructive pattern, decreased DLCO (<60% predicted)
chest CT scan
检查
Provides better visualization of type and distribution of lung tissue damage and bulla formation than chest x-ray. [Figure caption and citation for the preceding image starts]: COPD chest CT: hyperinflated lung, emphysematous changes, and increased antero-posterior diameter (barrel chest)From the collection of Manoochehr Abadian Sharifabad, MD [Citation ends].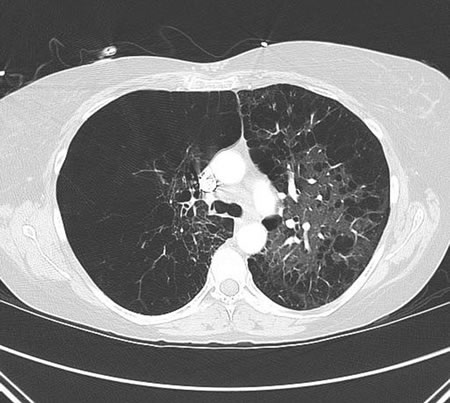
In contrast to smoking-related COPD, alpha-1 antitrypsin deficiency mainly affects lower fields.
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend consideration of CT scan for patients with persistent exacerbations, those with symptoms that do not correspond with disease severity on lung function testing, those with FEV₁ <45% of predicted with significant hyperinflation, and those meeting criteria for lung cancer screening.[1]
Annual low-dose CT scan (LDCT) is recommended by the US Preventive Services Task Force for lung cancer screening in patients with COPD that is due to smoking.[72]
结果
hyperinflation
serial peak flow measurement
检查
May be used to exclude asthma if there is diagnostic uncertainty.[2]
结果
<20% diurnal or day-to-day variability
sputum culture
检查
In patients with frequent exacerbations, severe airflow limitation, and/or exacerbations requiring mechanical ventilation, sputum should be sent for culture.[1]
结果
infecting organism
alpha-1 antitrypsin level
检查
Low level in patients with alpha-1 antitrypsin deficiency. Test is done if there is high suspicion for alpha-1 antitrypsin deficiency, such as a positive family history and atypical COPD cases (young patients [<45 years] and nonsmokers).[1] All patients with a diagnosis of COPD should be screened once, especially in areas with high prevalence of alpha-1 antitrypsin deficiency.[70][71]
结果
should be normal in patients with COPD that is related to smoking
exercise testing
检查
Can be of value in patients with a disproportional degree of dyspnea compared with spirometry.[1] It can be performed on a cycle or treadmill ergometer, or by a simple timed walking test (e.g., 6 minutes, or duration <6 minutes).[74] Exercise testing is of use in selecting patients for rehabilitation.
结果
poor exercise performance or exertional hypoxemia is suggestive of advanced disease
sleep study
检查
Obstructive sleep apnea, a common finding in patients with COPD, is associated with increased risk of death and hospitalization in patients with COPD.[73]
结果
elevated apnea-hypopnea index and/or nocturnal hypoxemia
respiratory muscle function
检查
Respiratory muscle function may be tested if dyspnea or hypercapnia are disproportionately increased with respect to FEV₁, as well as in patients with poor nutrition and those with corticosteroid myopathy.[75]
结果
reduced maximal inspiratory pressure
ECG
检查
Risk factors for COPD are similar to those for ischemic heart disease, so comorbidity is common. Right-sided heart failure may develop in longstanding COPD (cor pulmonale).
结果
signs of right ventricular hypertrophy, arrhythmia, ischemia
echocardiogram
检查
To assess cardiac status if cardiac disease or pulmonary hypertension are suspected.[2]
结果
may be normal or may show right-sided heart failure and/or pulmonary hypertension
blood eosinophil count
检查
Blood eosinophil counts can identify patients who are more likely to respond to inhaled corticosteroids (ICS).[76][77][78] They may predict the effectiveness of adding ICS to regular long-acting bronchodilator treatment to prevent exacerbations.[77][78][79] Little or no effect is seen with ICS at blood eosinophil counts of <100 cells/microliter, while maximal effect is seen at blood eosinophil counts of ≥300 cells/microliter.[76][80] These thresholds indicate approximate cut-off values that may help clinicians predict the likelihood of ICS treatment benefit.[1] Patients with blood eosinophils ≥300 cells/microliter are at greatest risk of exacerbations after withdrawing ICS.[81]
结果
may be normal or increased
内容使用需遵循免责声明


