History
COPD has an insidious onset and usually presents in older people. A history of productive cough, wheezing, and shortness of breath, particularly with exercise, is typical. Other symptoms include frequent bronchitis, reduced exercise tolerance, waking at night with breathlessness, ankle swelling, and fatigue.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
[2]National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication].
https://www.nice.org.uk/guidance/ng115
Patients may complain of fatigue as a result of disrupted sleep secondary to constant nocturnal cough and persistent hypoxia and hypercapnia. The patient's smoking history, occupational exposures, comorbidities, and any family history of lung disease should be determined. A history of previous exacerbations and hospitalisations should be sought.
Patients with COPD may also present with acute, severe shortness of breath, fever, and chest pain during acute infectious exacerbation. See Acute exacerbation of chronic obstructive pulmonary disease.
Physical examination
A physical examination is not diagnostic of COPD but is an important part of patient care.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
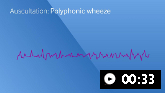
Examination may show tachypnoea, respiratory distress, use of accessory muscles, and intercostal retraction. Barrel chest is a common observation. There may be hyper-resonance on percussion, and distant breath sounds and poor air movement on auscultation. Wheezing, coarse crackles, clubbing, and cyanosis, as well as signs of right-sided heart failure (distended neck veins, loud P2, hepatomegaly, hepatojugular reflux, and lower-extremity oedema), may be present. Occasionally patients may exhibit asterixis - loss of postural control in the outstretched arms (commonly known as a flap) caused by hypercapnia. This is due to impaired gas exchange in lung parenchyma, worsens with exercise, and is suggestive of respiratory failure.
Initial tests
Spirometry is required to make the diagnosis of COPD and is also used for monitoring disease progress.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
[2]National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication].
https://www.nice.org.uk/guidance/ng115
[66]Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011 Aug 2;155(3):179-91.
https://www.acpjournals.org/doi/10.7326/0003-4819-155-3-201108020-00008
http://www.ncbi.nlm.nih.gov/pubmed/21810710?tool=bestpractice.com
It is the most reproducible and objective measure of airflow limitation. Spirometry should be performed after administering an adequate dose of at least one short-acting inhaled bronchodilator to minimise variability.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Patients with COPD have a distinctive pattern seen on spirometry, with a reduced FEV₁ and FEV₁/FVC ratio. The presence of airflow limitation is defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria as a post-bronchodilator FEV₁/FVC <0.7.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
In cases where FVC may be hard to measure, forced expiratory volume at 6 seconds (FEV₆) can be used.[67]Jing JY, Huang TC, Cui W, et al. Should FEV1/FEV6 replace FEV1/FVC ratio to detect airway obstruction? A metaanalysis. Chest. 2009 Apr;135(4):991-8.
http://www.ncbi.nlm.nih.gov/pubmed/19349398?tool=bestpractice.com
Spirometry also indicates the severity of airflow obstruction. In patients with an FEV₁/FVC ratio <0.7:[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
FEV₁ ≥80% predicted indicates mild COPD (GOLD 1)
FEV₁ <80% and ≥50% predicted indicates moderate COPD (GOLD 2)
FEV₁ <50% and ≥30% predicted indicates severe COPD (GOLD 3)
FEV₁ <30% predicted indicates very severe COPD (GOLD 4).
Chest x-ray is rarely diagnostic but should be performed to exclude other diagnoses and to assess for the presence of significant comorbidities.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
[68]American College of Radiology. ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin. 2024 [internet publication].
https://acsearch.acr.org/docs/69448/Narrative
Pulse oximetry screens for hypoxia and should be performed in all patients presenting with signs of respiratory failure or right heart failure. If peripheral arterial oxygen saturation is ≤92%, then arterial blood gases should be measured.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
In addition to airflow limitation, the GOLD guidelines recognise the importance of exacerbations in affecting the natural course of COPD, and place emphasis on assessment of symptoms, risk factors for exacerbations, and comorbidities.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
The Modified British Medical Research Council (mMRC) questionnaire or the COPD Assessment Test (CAT) are recommended to assess symptoms. GOLD cautions against the use of the mMRC dyspnoea scale alone for assessing patients, as symptoms of COPD go beyond dyspnoea alone. For this reason, the CAT is preferred. However, GOLD acknowledges that the use of the mMRC scale is widespread, and so a threshold of an mMRC grade ≥2 is still included to define 'more breathless' patients, as opposed to 'less breathless' patients, in its assessment criteria.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
The best predictor of frequent exacerbations (two or more per year) is a history of previously treated exacerbations.[69]Hurst JR, Vestbo J, Anzueto A, et al; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010 Sep 16;363(12):1128-38.
https://www.nejm.org/doi/full/10.1056/NEJMoa0909883
http://www.ncbi.nlm.nih.gov/pubmed/20843247?tool=bestpractice.com
The GOLD guidelines uses a combined 'ABE' approach to assess patients according to their level of symptoms and previous history of exacerbations. Symptoms are assessed using the mMRC or CAT scale. Exacerbations are assessed independently of symptoms to highlight their clinical relevance.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Group A: low risk (0-1 exacerbations per year, not requiring hospitalisation) and fewer symptoms (mMRC 0-1 or CAT <10)
Group B: low risk (0-1 exacerbations per year, not requiring hospitalisation) and more symptoms (mMRC ≥2 or CAT ≥10)
Group E: high risk (≥2 exacerbations per year, or ≥1 requiring hospitalisation) and any level of symptoms.
UK guidelines recommend a full blood count (FBC) for all newly diagnosed patients to screen for anaemia or polycythaemia.[2]National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication].
https://www.nice.org.uk/guidance/ng115
Other tests
Detailed pulmonary function tests performed in specialist pulmonary function laboratories can measure flow volume loops and inspiratory capacity. They are not used routinely but can be helpful in resolving diagnostic uncertainties and for preoperative assessment. Diffusing capacity of the lung for carbon monoxide (DLCO) was previously only measured in specialist laboratories; however, portable systems are now available, allowing measurements to be taken in the field. International guidelines from GOLD recommend a DLCO measurement if a patient with COPD has dyspnoea that is disproportionate to their degree of airflow obstruction. A low DLCO value (<60% predicted) in a patient with COPD is associated with decreased exercise capacity, worse health status, and increased risk of death.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Serial peak flow measurements may distinguish COPD from asthma if there is diagnostic uncertainty.[2]National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication].
https://www.nice.org.uk/guidance/ng115
In young patients (<45 years) with a family history or with rapidly progressing disease and lower lobe changes on imaging tests, alpha-1 antitrypsin level should be checked.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
All patients with a diagnosis of COPD should be screened once, especially in areas with high prevalence of alpha-1 antitrypsin deficiency.[70]World Health Organization. Alpha 1-antitrypsin deficiency: memorandum from a WHO meeting. Bull World Health Organ. 1997;75(5):397-415.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2487011/pdf/bullwho00396-0013.pdf
http://www.ncbi.nlm.nih.gov/pubmed/9447774?tool=bestpractice.com
[71]Miravitlles M, Dirksen A, Ferrarotti I, et al. European Respiratory Society statement: diagnosis and treatment of pulmonary disease in α(1)-antitrypsin deficiency. Eur Respir J. 2017 Nov;50(5).
https://www.doi.org/10.1183/13993003.00610-2017
http://www.ncbi.nlm.nih.gov/pubmed/29191952?tool=bestpractice.com
This may aid in family screening and counselling.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
GOLD guidelines recommend consideration of computed tomography (CT) scan for patients with persistent exacerbations, those with symptoms that do not correspond with disease severity on lung function testing, those with FEV₁ <45% of predicted with significant hyperinflation, and those meeting criteria for lung cancer screening.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Annual low-dose CT scan (LDCT) is recommended by the US Preventive Services Task Force (USPSTF) for lung cancer screening in patients with COPD that is due to smoking.[72]Krist AH, Davidson KW, Mangione CM, et al; US Preventive Services Task Force. Screening for lung cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021 Mar 9;325(10):962-70.
https://jamanetwork.com/journals/jama/fullarticle/2777244
http://www.ncbi.nlm.nih.gov/pubmed/33687470?tool=bestpractice.com
Obstructive sleep apnoea is associated with increased risk of death and hospitalisation in patients with COPD, and a sleep study should be considered.[73]Marin JM, Soriano JB, Carrizo SJ, et al. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010 Aug 1;182(3):325-31.
https://www.atsjournals.org/doi/10.1164/rccm.200912-1869OC
http://www.ncbi.nlm.nih.gov/pubmed/20378728?tool=bestpractice.com
Exercise testing can be useful in patients with a disproportional degree of dyspnoea.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
It can be performed on a cycle or treadmill ergometer, or by a simple timed walking test (e.g., 6 minutes, or duration <6 minutes).[74]Johnston KN, Potter AJ, Phillips A. Measurement properties of short lower extremity functional exercise tests in people with chronic obstructive pulmonary disease: systematic review. Phys Ther. 2017 Sep 1;97(9):926-43.
https://academic.oup.com/ptj/article/97/9/926/3866635
http://www.ncbi.nlm.nih.gov/pubmed/28605481?tool=bestpractice.com
Exercise testing is also of use in selecting patients for rehabilitation. Respiratory muscle function may also be tested if dyspnoea or hypercapnia are disproportionately increased with respect to FEV₁, as well as in patients with poor nutrition and those with corticosteroid myopathy.[75]Siafakas NM, Vermeire P, Pride NB, et al. Optimal assessment and management of chronic obstructive pulmonary disease (COPD). The European Respiratory Society Task Force. Eur Respir J. 1995 Aug;8(8):1398-420.
https://erj.ersjournals.com/content/erj/8/8/1398.full.pdf
http://www.ncbi.nlm.nih.gov/pubmed/7489808?tool=bestpractice.com
In patients with frequent exacerbations, severe airflow limitation, and/or exacerbations requiring mechanical ventilation, sputum should be sent for culture.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Risk factors for COPD are similar to those for ischaemic heart disease, so comorbidity is common. ECG may detect right ventricular hypertrophy, arrhythmia, or ischaemia. Echocardiogram evaluates suspected cardiac disease or pulmonary hypertension.[2]National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication].
https://www.nice.org.uk/guidance/ng115
The WHO has specified a minimum set of interventions for the diagnosis of COPD in primary care.
WHO: package of essential noncommunicable (PEN) disease interventions for primary health care
Opens in new window
Presence of high circulatory eosinophils predicts higher risk of exacerbations and predicts good response in preventative and therapeutic effects of corticosteroids. Blood eosinophil counts can identify patients who are more likely to respond to inhaled corticosteroids (ICS).[76]Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018 Feb;6(2):117-26.
http://www.ncbi.nlm.nih.gov/pubmed/29331313?tool=bestpractice.com
[77]Harries TH, Rowland V, Corrigan CJ, et al. Blood eosinophil count, a marker of inhaled corticosteroid effectiveness in preventing COPD exacerbations in post-hoc RCT and observational studies: systematic review and meta-analysis. Respir Res. 2020 Jan 3;21(1):3.
https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-019-1268-7
http://www.ncbi.nlm.nih.gov/pubmed/31900184?tool=bestpractice.com
[78]Oshagbemi OA, Odiba JO, Daniel A, et al. Absolute blood eosinophil counts to guide inhaled corticosteroids therapy among patients with COPD: systematic review and meta-analysis. Curr Drug Targets. 2019;20(16):1670-9.
http://www.ncbi.nlm.nih.gov/pubmed/31393244?tool=bestpractice.com
They may predict the effectiveness of adding ICS to regular long-acting bronchodilator treatment to prevent exacerbations.[77]Harries TH, Rowland V, Corrigan CJ, et al. Blood eosinophil count, a marker of inhaled corticosteroid effectiveness in preventing COPD exacerbations in post-hoc RCT and observational studies: systematic review and meta-analysis. Respir Res. 2020 Jan 3;21(1):3.
https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-019-1268-7
http://www.ncbi.nlm.nih.gov/pubmed/31900184?tool=bestpractice.com
[78]Oshagbemi OA, Odiba JO, Daniel A, et al. Absolute blood eosinophil counts to guide inhaled corticosteroids therapy among patients with COPD: systematic review and meta-analysis. Curr Drug Targets. 2019;20(16):1670-9.
http://www.ncbi.nlm.nih.gov/pubmed/31393244?tool=bestpractice.com
[79]Pascoe S, Barnes N, Brusselle G, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019 Sep;7(9):745-56.
http://www.ncbi.nlm.nih.gov/pubmed/31281061?tool=bestpractice.com
Little or no effect is seen with ICS at blood eosinophil counts of <100 cells/microlitre, while maximal effect is seen at blood eosinophil counts of ≥300 cells/microlitre.[76]Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018 Feb;6(2):117-26.
http://www.ncbi.nlm.nih.gov/pubmed/29331313?tool=bestpractice.com
[80]Cazzola M, Rogliani P, Calzetta L, et al. Triple therapy versus single and dual long-acting bronchodilator therapy in COPD: a systematic review and meta-analysis. Eur Respir J. 2018 Dec 13;52(6):1801586.
https://erj.ersjournals.com/content/52/6/1801586
http://www.ncbi.nlm.nih.gov/pubmed/30309975?tool=bestpractice.com
These thresholds indicate approximate cut-off values that may help clinicians predict the likelihood of ICS treatment benefit.[1]Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 report. 2025 [internet publication].
https://goldcopd.org/2025-gold-report
Patients with blood eosinophils ≥300 cells/microlitre are at greatest risk of exacerbations after withdrawing ICS.[81]Chapman KR, Hurst JR, Frent SM, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018 Aug 1;198(3):329-39.
https://www.atsjournals.org/doi/10.1164/rccm.201803-0405OC
http://www.ncbi.nlm.nih.gov/pubmed/29779416?tool=bestpractice.com