Summary
Definition
History and exam
Key diagnostic factors
- presença de fatores de risco
- sintomas progressivos e prolongados
- cefaleias
- disfunção erétil
- testículos pequenos e moles
- ginecomastia
- amenorreia
- infertilidade
- atrofia da mama
- perda da libido
- fogacho
- diaforese
- ganho de peso
- fadiga
- anorexia
- náuseas
- vômitos
- fraqueza
- acuidade visual reduzida
- hemianopsia bitemporal
- apoplexia hipofisária
- diplopia
Other diagnostic factors
- adiposidade central elevada
- massa muscular reduzida
- constipação
- intolerância ao frio
- pele ressecada
- queda de cabelos
- dificuldades de memória
- humor deprimido
- osteopenia
- perda de peso
- nervosismo
- dormência facial
- desequilíbrio
- incontinência urinária
- sinusite recorrente
- bradicardia
- convulsões
Risk factors
- neoplasia endócrina múltipla tipo 1 (NEM-1)
- adenomas hipofisários familiares isolados (FIPA)
- complexo de Carney (CNC)
Diagnostic tests
1st tests to order
- prolactina
- fator de crescimento semelhante à insulina-1
- hormônio luteinizante, hormônio folículo-estimulante
- subunidade alfa de hormônios glicoproteicos hipofisários
- testosterona
- estradiol
- hormônio estimulante da tireoide, tiroxina livre
- cortisol matinal
- teste de estímulo com o hormônio adrenocorticotrófico (ACTH)
- hormônio adrenocorticotrófico
- teste de tolerância à insulina para cortisol
- perfil metabólico básico
- Hemograma completo
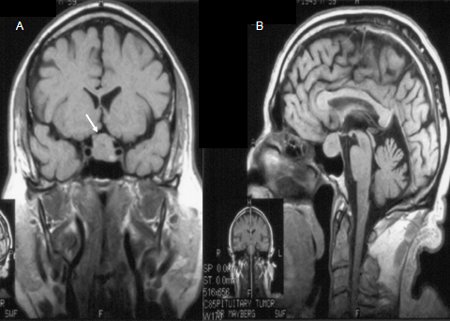
- ressonância nuclear magnética (RNM) da hipófise com contraste de gadolínio
- TC com contraste da hipófise
Tests to consider
- teste de estímulo do hormônio do crescimento
- perfil lipídico
- teste formal do campo visual de Humphrey ou Goldmann
- coloração imuno-histoquímica
Treatment algorithm
apoplexia hipofisária
microadenoma
macroadenoma sem efeito de massa e não contíguo ao quiasma óptico
macroadenoma sem efeito de massa, mas contíguo ao quiasma óptico
macroadenoma com efeito de massa
Contributors
Authors
Susmeeta Tewari Sharma, MD, MBBS, MHSc
Director of Pituitary Endocrinology
MedStar Washington Hospital Center/Georgetown University Hospital
Washington
DC
Disclosures
STS declares that she has no competing interests.
Acknowledgements
Dr Susmeeta Tewari Sharma would like to gratefully acknowledge Dr Gabriel Zada, Dr John Carmichael, Dr Israel Orija and Dr Amir H. Hamrahian, previous contributors to this topic. GZ, JC, IO and AH declare that they have no competing interests.
Peer reviewers
S. Bulent Omay, MD
Assistant Professor of Neurosurgery
Yale Medical School
New Haven
CT
Disclosures
SBO declares that he has no competing interests.
Andrew James, BSc, MB BCh, MD, MRCP, FRCP
Consultant Endocrinologist
Newcastle Hospitals NHS Foundation Trust
Royal Victoria Infirmary
Newcastle
UK
Disclosures
AJ declares that he has no competing interests.
Federico Roncaroli, MD
Reader in Neuropathology and Honorary Consultant in Neuropathology
Neuropathology Unit
Department of Clinical Neuroscience
Division of Neuroscience and Mental Health
Faculty of Medicine
Imperial College
London
UK
Disclosures
FR declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Molitch ME. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017 Feb 7;317(5):516-24. Abstract
Mercado M, Melgar V, Salame L, et al. Clinically non-functioning pituitary adenomas: pathogenic, diagnostic and therapeutic aspects. [in spa]. Endocrinol Diabetes Nutr. 2017 Aug-Sep;64(7):384-95. Abstract
Aghi MK, Chen CC, Fleseriu M, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the management of patients with nonfunctioning pituitary adenomas: executive summary. Neurosurgery. 2016 Oct;79(4):521-3.Full text Abstract
Esposito D, Olsson DS, Ragnarsson O, et al. Non-functioning pituitary adenomas: indications for pituitary surgery and post-surgical management. Pituitary. 2019 Aug;22(4):422-34.Full text Abstract
Minniti G, Flickinger J. The risk/benefit ratio of radiotherapy in pituitary tumors. Best Pract Res Clin Endocrinol Metab. 2019 Apr;33(2):101269. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Adenoma secretor de prolactina (prolactinoma)
- Adenoma secretor de hormônio do crescimento (acromegalia)
- Adenoma secretor de hormônio adrenocorticotrófico (síndrome de Cushing)
More DifferentialsGuidelines
- Suspected cancer: recognition and referral
- Clinical practice guideline on functioning and nonfunctioning pituitary adenomas in pregnancy
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer
