Approach
The diagnostic approach to measles begins with obtaining a history of potential exposures and risk factors, performing a detailed physical examination, applying clinical definitions, and obtaining, if necessary, laboratory tests to confirm the diagnosis. Where measles is common, the diagnosis is clinical. In regions where measles is rare, confirmation of the diagnosis by laboratory testing has become the norm. Although a clinical case definition has been developed for epidemiologic purposes, measles can be difficult to distinguish from other febrile exanthems such as rubella, roseola, dengue, erythema infectiosum (parvovirus B19), EBV infection, zika virus infection, and drug eruptions.
Clinical features
Typical clinical features include fever with an erythematous exanthem of acute onset following a 2 to 4 day prodrome with cough, coryza, conjunctivitis, and irritability. More specific features include presence of Koplik spots (classically described as red spots with a white central dot on erythematous buccal mucosa), progression of rash from head to torso and extremities, and resolution of fever soon after appearance of the rash.[Figure caption and citation for the preceding image starts]: Koplik spotsCenters for Disease Control and Prevention [Citation ends].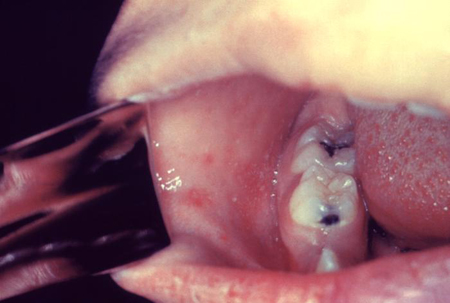 [Figure caption and citation for the preceding image starts]: Koplik spotsCenters for Disease Control and Prevention [Citation ends].
[Figure caption and citation for the preceding image starts]: Koplik spotsCenters for Disease Control and Prevention [Citation ends]. [Figure caption and citation for the preceding image starts]: Close-up view of the measles rash on day 3Centers for Disease Control and Prevention [Citation ends].
[Figure caption and citation for the preceding image starts]: Close-up view of the measles rash on day 3Centers for Disease Control and Prevention [Citation ends].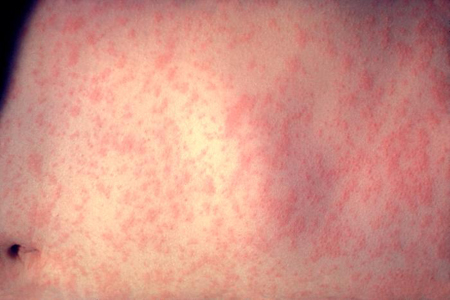 [Figure caption and citation for the preceding image starts]: Child with measles showing the characteristic red blotchy rash on his buttocks and back during the third day of the rashCenters for Disease Control and Prevention [Citation ends].
[Figure caption and citation for the preceding image starts]: Child with measles showing the characteristic red blotchy rash on his buttocks and back during the third day of the rashCenters for Disease Control and Prevention [Citation ends].
The clinical case definition of measles is presence of rash lasting 3 or more days, temperature of 101°F (38.3°C) or higher, cough, conjunctivitis, or coryza.[30] This definition, however, is used mostly for epidemiologic purposes and its use for clinical diagnosis is limited by the fact that rash lasting 3 days is required, and other viral exanthems can also meet this case definition.
Diagnostic tests
The most commonly used diagnostic test is detection of measles-specific IgM antibody.[31] In primary infection this antibody appears within a few days of onset of rash. Sensitivity is highest 3 to 14 days after rash onset.[32]
Enzyme-linked immunosorbent assays (ELISAs) that detect measles-specific IgM and IgG in serum are widely used as they are sensitive and easy to perform. Sensitivity (83% to 92%) and specificity (87% to 100%) are good.[33] Rubella and parvovirus B19 infection may cause false-positive IgM ELISAs.
Serum samples are used for IgM/IgG detection in the US and measles RNA can be detected by polymerase chain reaction (PCR) from throat or nasopharyngeal swabs or from urine samples.[31] Best yield is obtained when samples are collected on days 1 to 3 of the rash, but virus still may be detected up to 10 to 14 days after rash onset.[34]
Paired sera (acute and convalescent) can be used to detect a 4-fold rise in IgG antibody by complement fixation, hemagglutination inhibition, and neutralization.[31]
The plaque reduction neutralization test has remained the definitive test against which other test methods are measured, but it is labor-intensive and its use is limited to research laboratories.
Antigen detection by fluorescent antibody testing and virus isolation in tissue culture systems is available, but these are more labor-intensive processes and generally are limited to research labs.
Use of this content is subject to our disclaimer
