小结
定义
病史和体格检查
危险因素
- exposure to infection
- birth in an endemic country
- HIV infection
- immunosuppressive drugs
- malignancy
- silicosis
- end-stage renal disease
- apical fibrosis
- intravenous drug use
- malnutrition
- alcoholism
- diabetes
- high-risk congregate settings
- low socioeconomic status or black/Hispanic/Native-American ancestry
- age
- tobacco smoking
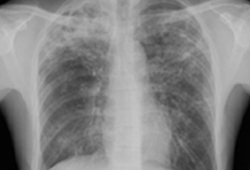
诊断性检查
治疗流程
撰稿人
作者
David J. Horne, MD, MPH

Associate Professor
Division of Pulmonary, Critical Care, and Sleep Medicine
Department of Medicine
University of Washington
Seattle
WA
利益声明
DJH declares that he has no competing interests.
Masahiro Narita, MD
Professor of Medicine
Division of Pulmonary, Critical Care, and Sleep Medicine
Department of Medicine
University of Washington
Seattle
WA
利益声明
MN declares that he has no competing interests. MN is the author of a reference cited in this topic.
同行评议者
Fayez Kheir, MD, MSc
Assistant Professor of Medicine
Harvard Medical School
Division of Pulmonary and Critical Care
Massachusetts General Hospital
Boston
MA
利益声明
FK declares that he has no competing interests.
William Burman, MD
Professor
Division of Infectious Diseases
University of Colorado at Denver and Health Sciences Center
Denver
CO
利益声明
WB declares that he has no competing interests.
Ian Campbell, MD (Lond), FRCP (Edin & Lond)
Consultant Chest Physician
Llandough Hospital
Llandough
Penarth
South Wales
利益声明
IC declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
参考文献
关键文献
Nahid P, Dorman SE, Alipanah N, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016 Oct;63(7):e147-95.全文 摘要
Lewinsohn DM, Leonard MK, LoBue PA, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017 Jan 15;64(2):e1-33.全文 摘要
World Health Organization. WHO consolidated guidelines on tuberculosis: module 5: management of tuberculosis in children and adolescents. Mar 2022 [internet publication].全文
National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: mycobacterium tuberculosis infection and disease. 2024 [internet publication].全文
Nahid P, Mase SR, Migliori GB, et al. Treatment of drug-resistant tuberculosis. An official ATS/CDC/ERS/IDSA clinical practice guideline. Am J Respir Crit Care Med. 2019 Nov 15;200(10):e93-142.全文 摘要
World Health Organization. WHO consolidated guidelines on tuberculosis: module 4: treatment: drug-susceptible tuberculosis treatment. May 2022 [internet publication].全文
Uthman OA, Okwundu C, Gbenga K, et al. Optimal timing of antiretroviral therapy initiation for HIV-infected adults with newly diagnosed pulmonary tuberculosis: a systematic review and meta-analysis. Ann Intern Med. 2015 Jul 7;163(1):32-9. 摘要
World Health Organization. WHO consolidated guidelines on tuberculosis: module 4: treatment: drug-resistant tuberculosis treatment, 2022 update. Dec 2022 [internet publication].全文
Tuberculosis Trials Consortium. Rifapentine and isoniazid once a week versus rifampicin and isoniazid twice a week for treatment of drug-susceptible pulmonary tuberculosis in HIV-negative patients: a randomised clinical trial. Lancet. 2002 Aug 17;360(9332):528-34. 摘要
American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America. Controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005 Nov 1;172(9):1169-227.全文 摘要
参考文献
A full list of sources referenced in this topic is available here.
内容使用需遵循免责声明