Summary
Definition
History and exam
Key diagnostic factors
- longstanding and progressing symptoms
- headaches
- erectile dysfunction
- soft small testicles
- gynecomastia
- amenorrhea
- infertility
- breast atrophy
- loss of libido
- hot flashes
- diaphoresis
- weight gain
- fatigue
- anorexia
- nausea
- vomiting
- weakness
- decreased visual acuity
- bitemporal hemianopia
- pituitary apoplexy
- diplopia
Other diagnostic factors
- increased central adiposity
- reduced muscle mass
- constipation
- cold intolerance
- dry skin
- hair loss
- poor memory
- low mood
- osteopenia
- weight loss
- nervousness
- facial numbness
- imbalance
- urinary incontinence
- recurrent sinusitis
- bradycardia
- seizures
Risk factors
- multiple endocrine neoplasia type 1 (MEN-1)
- familial isolated pituitary adenomas (FIPA)
- Carney complex (CNC)
Diagnostic investigations
1st investigations to order
- prolactin
- insulin-like growth factor 1
- luteinising hormone, follicle-stimulating hormone
- alpha subunit of human pituitary glycoprotein hormones
- testosterone
- estradiol
- thyroid-stimulating hormone, free thyroxine
- morning cortisol
- adrenocorticotropic hormone stimulation test
- adrenocorticotropic hormone
- insulin tolerance test for cortisol
- basic metabolic panel
- CBC
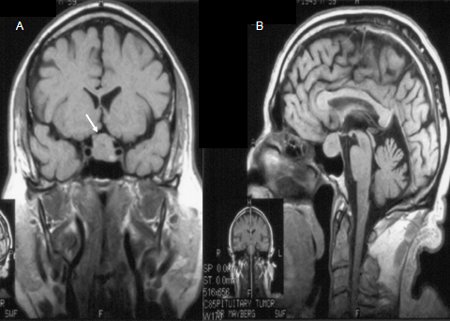
- MRI pituitary with gadolinium enhancement
- contrast-enhanced CT pituitary
Investigations to consider
- growth hormone stimulation test
- lipid panel
- Humphrey or Goldmann formal visual fields test
- immunohistochemical staining
Treatment algorithm
pituitary apoplexy
microadenoma
macroadenoma without mass effect and not abutting optic chiasm
macroadenoma without mass effect but abutting optic chiasm
macroadenoma with mass effect
Contributors
Authors
Susmeeta Tewari Sharma, MD, MBBS, MHSc
Director of Pituitary Endocrinology
MedStar Washington Hospital Center/Georgetown University Hospital
Washington
DC
Disclosures
STS declares that she has no competing interests.
Acknowledgements
Dr Susmeeta Tewari Sharma would like to gratefully acknowledge Dr Gabriel Zada, Dr John Carmichael, Dr Israel Orija and Dr Amir H. Hamrahian, previous contributors to this topic. GZ, JC, IO and AH declare that they have no competing interests.
Peer reviewers
S. Bulent Omay, MD
Assistant Professor of Neurosurgery
Yale Medical School
New Haven
CT
Disclosures
SBO declares that he has no competing interests.
Andrew James, BSc, MB BCh, MD, MRCP, FRCP
Consultant Endocrinologist
Newcastle Hospitals NHS Foundation Trust
Royal Victoria Infirmary
Newcastle
UK
Disclosures
AJ declares that he has no competing interests.
Federico Roncaroli, MD
Reader in Neuropathology and Honorary Consultant in Neuropathology
Neuropathology Unit
Department of Clinical Neuroscience
Division of Neuroscience and Mental Health
Faculty of Medicine
Imperial College
London
UK
Disclosures
FR declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Molitch ME. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017 Feb 7;317(5):516-24. Abstract
Mercado M, Melgar V, Salame L, et al. Clinically non-functioning pituitary adenomas: pathogenic, diagnostic and therapeutic aspects. [in spa]. Endocrinol Diabetes Nutr. 2017 Aug-Sep;64(7):384-95. Abstract
Aghi MK, Chen CC, Fleseriu M, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the management of patients with nonfunctioning pituitary adenomas: executive summary. Neurosurgery. 2016 Oct;79(4):521-3.Full text Abstract
Esposito D, Olsson DS, Ragnarsson O, et al. Non-functioning pituitary adenomas: indications for pituitary surgery and post-surgical management. Pituitary. 2019 Aug;22(4):422-34.Full text Abstract
Minniti G, Flickinger J. The risk/benefit ratio of radiotherapy in pituitary tumors. Best Pract Res Clin Endocrinol Metab. 2019 Apr;33(2):101269. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Prolactin-secreting adenoma (prolactinoma)
- Growth hormone-secreting adenoma (acromegaly)
- Adrenocorticotropic hormone-secreting adenoma (Cushing syndrome)
More DifferentialsGuidelines
- Clinical practice guideline on functioning and nonfunctioning pituitary adenomas in pregnancy
- Appropriateness Criteria: neuroendocrine imaging
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer