Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- cough with increasing sputum production
- fever or chills
- dyspnea
- pleuritic pain
- abnormal auscultatory findings
Fatores de risco
- age >65 years
- residence in a healthcare setting
- COPD
- exposure to cigarette smoke
- alcohol abuse
- poor oral hygiene
- use of acid-reducing drugs, inhaled corticosteroids, antipsychotics, antidiabetic drugs
- contact with children
- HIV infection
- diabetes mellitus
- chronic renal disease
- chronic liver disease
- use of opioids
Investigações diagnósticas
Primeiras investigações a serem solicitadas
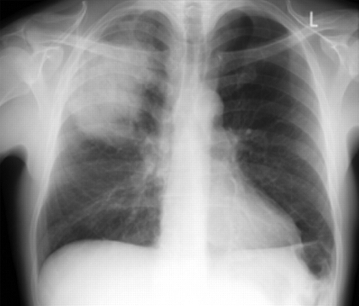
- chest x-ray
- CBC
- serum electrolytes/blood urea nitrogen
- liver function tests
- blood glucose
- arterial blood gases/oximetry
- blood culture
- sputum culture
Investigações a serem consideradas
- point-of-care lung ultrasound
- CT chest
- urinary antigen testing for Legionella and pneumococcus
- serum C-reactive protein
- serum procalcitonin
- thoracocentesis and pleural fluid culture
- bronchoscopy
- tests for respiratory viruses
- molecular microbiological techniques
Algoritmo de tratamento
Colaboradores
Consultores especialistas
Catia Cilloniz, MD, PhD, FERS
Applied Research in Respiratory Diseases
Hospital Clinic of Barcelona
CIBERES
IDIBAPS
Associate Professor
University of Barcelona
Barcelona
Spain
Declarações
CC is an author of a number of references cited in this topic.
Antoni Torres, MD, PhD
Professor of Medicine
Director
Pulmonary Intensive Care Unit
Respiratory Institute
Hospital Clinic of Barcelona
Barcelona
Spain
Declarações
AT is an author of a number of references cited in this topic.
Revisores
Barbara Jones, MD, MSc
Assistant Professor
Division of Pulmonary and Critical Care Medicine
University of Utah
Salt Lake City
UT
Declarações
BJ declares that she has no competing interests.
Denise Nassisi, MD
Associate Professor
Departments of Emergency Medicine and Medicine
Icahn School of Medicine at Mount Sinai
New York
NY
Declarações
DN declares that she has no competing interests.
Jeremy Brown, MBBS, FRCP, PhD
Professor of Respiratory Infection/Honorary Consultant
University College London
London
UK
Declarações
JB was a member of the NICE pneumonia guidelines committee.
Grant Waterer, MBBS, PhD, MBA, FRACP, FCCP
Professor of Medicine
Royal Perth Hospital
Perth
Australia
Declarações
GW declares that he has no competing interests.
Nathan Dean, MD
Professor (clinical) of Medicine
Section Chief Pulmonary Critical Care Medicine
University of Utah
Intermountain Medical Center
Murray
UT
Declarações
ND declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-67.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível aqui.
Use of this content is subject to our disclaimer