Summary
Definition
History and exam
Key diagnostic factors
- pain (e.g., abdomen, chest, bone)
- family history of cancer
- constitutional symptoms
Other diagnostic factors
- jaundice
- symptoms of post-obstructive pneumonia
- haemoptysis
- ascites
- cervical chain adenopathy
- personal history of previous cancer
- history of smoking
- palpable mass
- neuropathic pain or weakness
- headaches
- seizures
- delirium
- history of heavy alcohol consumption
- hepatomegaly
Risk factors
- age >60 years
Diagnostic investigations
1st investigations to order
- full blood count
- comprehensive metabolic panel
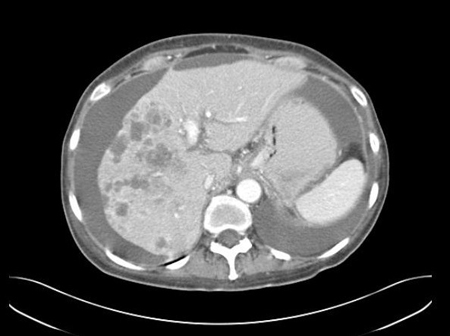
- CT chest/abdomen/pelvis
- MRI
- biopsy (pathological assessment)
- immunohistochemistry (IHC) tests
Investigations to consider
- fecal occult blood test
- lactate dehydrogenase
- urinalysis
- 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET)/CT
- breast imaging (mammography, MRI, ultrasound)
- transvaginal ultrasound
- paracentesis
- endoscopy
- direct laryngoscopy with or without oesophagoscopy and bronchoscopy
- serum tumour markers
- genetic biomarker testing
Emerging tests
- tissue of origin testing
Treatment algorithm
identification of primary site pending
unfavourable subtype: multiple metastases and/or without a likely primary site
favourable subtype: women with isolated axillary lymphadenopathy (likely breast primary)
favourable subtype: women with peritoneal carcinomatosis of a serous papillary adenocarcinoma (likely ovarian primary)
favourable subtype: poorly differentiated carcinoma with neuroendocrine features (likely small cell lung cancer primary)
favourable subtype: well-differentiated neuroendocrine tumours (likely neuroendocrine primary)
favourable subtype: adenocarcinoma with colorectal immunohistochemistry (likely colorectal primary)
favourable subtype: poorly differentiated carcinoma of the mediastinum or retroperitoneum in males <40 years (likely testicular primary)
favourable subtype: blastic bone metastases with immunohistochemistry/serum prostate-specific antigen (likely prostate primary)
favourable subtype: single metastatic lesion
favourable subtype: oligometastatic disease
Contributors
Authors
Michael S. Lee, MD
Associate Professor
Department of Gastrointestinal Medical Oncology
Division of Cancer Medicine
University of Texas MD Anderson Cancer Center
Houston
TX
Disclosures
MSL has consulted for Pfizer, Bayer, Delcath, and Imvax. His institution has received research funding from Amgen, Exelixis, Bristol-Myers Squibb, Pfizer, Rafael Pharmaceuticals, EMD Serono, Genentech/Roche, Merck, Arcus, and Shanghai EpiMab Biotherapeutics. MSL is the author of a number of papers cited in this topic.
Acknowledgements
Dr Michael S. Lee would like to gratefully acknowledge Dr Ross C. Donehower, Dr David Cosgrove, and Dr Hatim Hussain, previous contributors to this topic.
Disclosures
RCD, DC, and HH declare that they have no competing interests.
Peer reviewers
Nikhil Khushalani, MD
Assistant Professor
Department of Medicine
Roswell Park Cancer Institute
Buffalo
NY
Disclosures
NK declares that he has no competing interests.
Zelig Tochner, MD
Associate Professor
Radiation Oncology
Children's Hospital of Philadelphia
Philadelphia
PA
Disclosures
ZT declares that he has no competing interests.
Justin Stebbing, MA, MRCP, MRCPath, PhD
Consultant Medical Oncologist/Senior Lecturer
Department of Medical Oncology
Imperial College/Imperial Healthcare NHS Trust
Charing Cross Hospital
London
UK
Disclosures
JS declares that he has no competing interests.
References
Key articles
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: occult primary [internet publication].Full text
Krämer A, Bochtler T, Pauli C, et al. Cancer of unknown primary: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023 Mar;34(3):228-46.Full text Abstract
National Institute for Health and Care Excellence. Metastatic malignant disease of unknown primary origin in adults: diagnosis and management. Apr 2023 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Squamous or neuroendocrine carcinoma of unknown primary
More DifferentialsGuidelines
- NCCN clinical practice guidelines in oncology: head and neck cancers
- NCCN clinical practice guidelines in oncology: occult primary
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer