Summary
Definition
History and exam
Key diagnostic factors
- mecanismo de lesão concordante
- dor cervical
- fatores de risco
Other diagnostic factors
- nível de consciência reduzido
- parestesia nos membros
- fraqueza motora
- perda sensitiva
- disfunção do intestino ou da bexiga
- priapismo
- deficit do nervo craniano
- sinal de Hoffman
- Sinal de Babinski
- choque neurogênico
- choque medular
Risk factors
- sexo masculino
- sexo feminino (lesão por chicote)
- 18-40 anos ou >65 anos
- um mecanismo de lesão perigoso
- lesões traumáticas que causam distração
- falta de preparo ou consciência da colisão
- cabeça rotacionada no momento da colisão
- trauma ou cirurgia da coluna cervical prévios
- anormalidade preexistente na espinha, crânio ou em outra parte do corpo
Diagnostic tests
1st tests to order
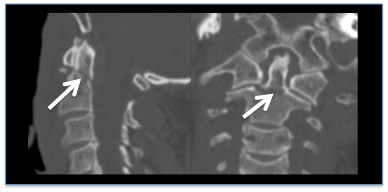
- TC de alta resolução da coluna cervical
Tests to consider
- TC da coluna vertebral inteira
- ressonância nuclear magnética (RNM) da coluna cervical
Treatment algorithm
suspeita de lesão da coluna cervical
lesão da coluna cervical confirmada
lesão por estiramento simples do pescoço ou efeito chicote
Contributors
Expert advisers
Dr Ram Hariharan, FRCP
Consultant
Yorkshire Regional Spinal Injuries Centre
Pinderfields Hospital
Aberford road
Mid Yorkshire Teaching Hospitals NHS Trust
Wakefield
UK
Disclosures
RH declares that he has no competing interests.
Acknowledgements
BMJ Best Practice would like to gratefully acknowledge the previous expert contributors, whose work has been retained in parts of the content:
Christopher S. Ahuja, MD
Research Fellow
Division of Neurosurgery
Department of Surgery
University of Toronto
Ontario
Canada
Michael G. Fehlings, MD, PhD, FRCS(C), FACS
Professor Division of Neurosurgery
Director of Neuroscience Program
University of Toronto
Krembil Chair in Neural Repair and Regeneration
Medical Director
Krembil Neuroscience Center
Toronto Western Hospital
Ontario
Canada
Muhammad Dherijha MBBS, MRCS
ST8 Neurosurgery
Health Education Northwest
Manchester Clinical Neuroscience Centre
Salford
UK
Declarações
CSA declares that he has no competing interests. MGF served as a consultant for Zimmer, In Vivo Therapeutics, and Pfizer. He receives institutional fellowship grant support from AOSpine, Medtronic, and Depuy-Synthes. MD declares that he has no competing interests.
Revisores
Jonathan Lucas, MBBS, FRCS (Eng), FRCS (Orth&Tr)
Head of Service - Paediatric Spinal and Orthopaedic Surgery
Consultant Spinal Surgeon
Guys and St Thomas’ NHS Foundation Trust
Evelina London Children’s Hospital
Guys Hospital
London
UK
Declarações
JL is an Education Consultant to Nuvasive Inc. in the subject of paediatric spinal deformity surgery.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Editores
Helena Delgado-Cohen
Section Editor, BMJ Best Practice
Declarações
HDC declares that she has no competing interests.
Susan Mayor
Lead Section Editor, BMJ Best Practice
Declarações
SM works as a freelance medical journalist and editor, video editorial director and presenter, and communications trainer. In this capacity, she has been paid, and continues to be paid, by a wide range of organisations for providing these skills on a professional basis. These include: NHS organisations, including the National Institute for Health and Care Excellence, NHS Choices, NHS Kidney Care, and others; publishers and medical education companies, including the BMJ Group, the Lancet group, Medscape, and others; professional organisations, including the British Thoracic Oncology Group, the European Society for Medical Oncology, the National Confidential Enquiry into Patient Outcome and Death, and others; charities and patients’ organisations, including the Roy Castle Lung Cancer Foundation and others; pharmaceutical companies, including Bayer, Boehringer Ingelheim, Novartis, and others; and communications agencies, including Publicis, Red Healthcare and others. She has no stock options or shares in any pharmaceutical or healthcare companies; however, she invests in a personal pension, which may invest in these types of companies. She is managing director of Susan Mayor Limited, the company name under which she provides medical writing and communications services.
Rachel Wheeler
Lead Section Editor, BMJ Best Practice
Declarações
RW declares that she has no competing interests.
Annabel Sidwell
Comorbidities Editor, BMJ Best Practice
Declarações
AS declares that she has no competing interests.
Adam Mitchell
Drug Editor, BMJ Best Practice
Declarações
AM declares that he has no competing interests.
Referências
Principais artigos
National Institute for Health and Care Excellence. Spinal injury: assessment and initial management. Feb 2016 [internet publication].Texto completo
National Institute for Health and Care Excellence. Spinal injury: assessment and initial management. Methods, evidence and recommendations. Feb 2016 [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Dor cervical não traumática
- Doença degenerativa da coluna cervical
- Torcicolo adquirido
Mais Diagnósticos diferenciaisGuidelines
- Head injury: assessment and early management
- Spinal injury: assessment and initial management
Mais GuidelinesCalculators
Escala de coma de Glasgow
More CalculatorsPatient information
Lesão por chicote
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer