Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- disfagia
Outros fatores diagnósticos
- postura para auxiliar na deglutição
- pressão/dor retroesternal
- regurgitação
- perda de peso gradual
- pirose
- alimentação lenta
- tosse/sufocamento na posição de decúbito
- infecções torácicas recorrentes
- sensação de nó na garganta (globus)
- soluços
Fatores de risco
- vírus do herpes e sarampo
- doença autoimune
- antígenos leucocitários humanos (HLA) classe II
- pais consanguíneos
- síndrome de Allgrove (triplo A)
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- endoscopia digestiva alta
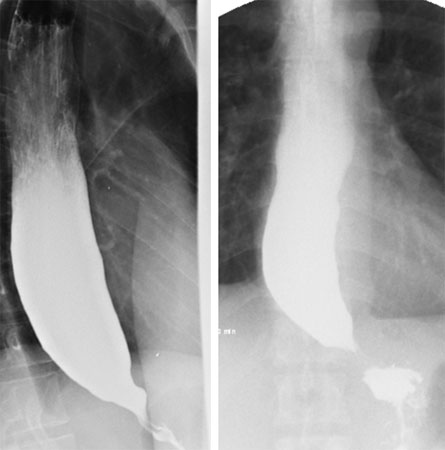
- esofagografia baritada
- manometria esofágica de alta resolução
Investigações a serem consideradas
- radiografia torácica
- estudos do esvaziamento esofágico por radionucleotídeos
- esofagograma com bário cronometrado
- tomografia computadorizada (TC) do tórax
- planimetria por impedância
Algoritmo de tratamento
pacientes que aguardam tratamento definitivo
bom candidato cirúrgico
não candidato à cirurgia
Colaboradores
Autores
Jamal Omar Hayat, MBBS, BSc, MRCP, MD (Res)
Consultant Gastroenterologist and Honorary Senior Lecturer
Department of Gastroenterology
St George's University Hospitals NHS Trust
London
UK
Declarações
JOH declares that he has no competing interests.
Kalliopi Alexandropoulou, MD, FRCP
Consultant Gastroenterologist
Royal Surrey County Hospital
Guildford
Surrey
UK
Declarações
KA declares that she has no competing interests.
Agradecimentos
Dr Jamal Omar Hayat and Dr Kalliopi Alexandropoulou wish to gratefully acknowledge Dr Jin-Yong Kang, the previous contributor to this topic.
Declarações
JYK declares that he has no competing interests.
Revisores
Nigel Trudgill, MB ChB
Consultant Gastroenterologist
Sandwell General Hospital
West Bromwich
UK
Declarações
NT declares that he has no competing interests.
John de Caestecker, BChir
Consultant in General Medicine
Leicester General Hospital
Leicester
UK
Declarações
JdC declares that he has no competing interests.
David Hackam, MD, PhD
Assistant Professor of Surgery
Children's Hospital of Pittsburgh
Pittsburgh
PA
Declarações
DH declares that he has no competing interests.
George Y. Wu, MD, PhD
Professor of Medicine
University of Connecticut Health Center
Farmington
CT
Declarações
GYW is on the medical advisory boards of the following: Gilead Sciences, Bristol-Myers Squibb, AbbVie, and Intercept.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus. 2018 Sep 1;31(9).Texto completo Resumo
Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020 Sep;115(9):1393-411.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Carcinoma esofágico
- Esofagite de refluxo
- Doenças do tecido conjuntivo (por exemplo, esclerose sistêmica)
Mais Diagnósticos diferenciaisDiretrizes
- Adverse events associated with EGD and EGD-related techniques
- Diagnosis and management of achalasia
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal