Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- frequência de pulso <50 bpm
- idade >70 anos
- uso de medicamentos causadores conhecidos
- presença de causa subjacente conhecida
- tontura
- síncope
- fadiga
- intolerância ao exercício
- dispneia
- ondas A em canhão em pulso venoso jugular
- estase jugular
Outros fatores diagnósticos
- pressão intracraniana elevada
- bulhas cardíacas anormais
- edema abdominal ou dos membros inferiores
- hipotensão
- alterações do estado mental
- palidez
- extremidades frias ao serem tocadas
- hipotermia
- dor torácica
- erupções cutâneas
- bócio tireoidiano
Fatores de risco
- uso de medicamentos causadores conhecidos
- idade >70 anos
- infarto do miocárdio recente
- cirurgia
- procedimentos de substituição da valva percutânea
- hipotireoidismo
- distúrbios eletrolíticos
- acidose
- infecções
- exposição a toxinas
- hipotermia
- doenças infiltrantes
- distúrbios respiratórios do sono
- epilepsia
Investigações diagnósticas
Primeiras investigações a serem solicitadas
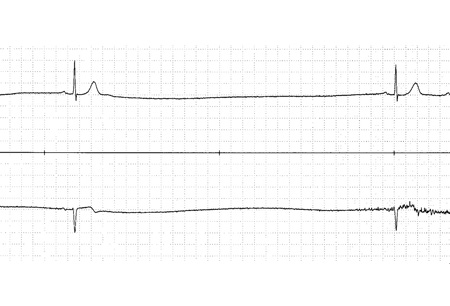
- eletrocardiograma (ECG) de 12 derivações
- monitoramento com Holter
- Monitoramento de evento/telemetria cardíaca móvel
- teste ergométrico
- massagem do seio carotídeo
- ecocardiograma
- testes da função tireoidiana
- perfil metabólico básico
- gasometria arterial
- biomarcadores cardíacos
- nível sérico de digoxina
- creatinina sérica
Investigações a serem consideradas
- loop event recorder implantável
- teste da mesa inclinável
- Títulos de Lyme
- teste eletrofisiológico
- oximetria de pulso noturna ou polissonografia noturna
Algoritmo de tratamento
hemodinamicamente instável
hemodinamicamente estável: disfunção do nó sinusal
hemodinamicamente estável: bloqueio atrioventricular adquirido
hemodinamicamente estável: bloqueio atrioventricular congênito
hemodinamicamente estável: bradicardia vagalmente mediada
hemodinamicamente estável: bradicardia associada a distúrbios neurológicos
Colaboradores
Autores
Brian Olshansky, MD, FAHA, FACC, FHRS, FESC

Professor Emeritus
University of Iowa
Iowa City
Adjunct Professor
Des Moines University
Electrophysiologist
Covenant Hospital
Waterloo
IA
VA Hospital
Iowa City
IA
CGH Medical Center
Sterling
IL
Declarações
BO declares that he has no competing interests.
Sandeep Saha, MD, MS, FACC, FHRS
Consultant, Cardiology and Cardiac Electrophysiology
Oregon Heart Center
Salem
OR
Declarações
SS is a consultant for Medtronic and St Jude Medical. He is on the speakers' bureau and serves as an advisory board member for Medtronic. None of these activities are relevant to the content of this topic.
Rakesh Gopinathannair, MD, MA, FAHA, FACC, FHRS

Director, Cardiac Electrophysiology Laboratories
Kansas City Heart Rhythm Institute and Research Foundation
EP Medical Director
Research Medical Center, HCA Midwest Health
Overland Park
KS
Clinical Professor of Medicine
University of Missouri-Columbia
Columbia
MO
Declarações
RG is a consultant for St. Jude Medical, Biotrionik, and Boston Scientific. He is on the speakers' bureau for Pfizer Inc. and Zoll Medical. He serves as a physician advisor for HealthTrust PG and AltaThera Pharma, and PaceMate. None of these activities are relevant to the content of this topic.
Agradecimentos
Professor Brian Olshansky, Dr. Sandeep Saha, and Professor Rakesh Gopinathannair would also like to acknowledge Dr Giselle Statz, Dr Renee M. Sullivan, Dr Weiwei Li, Dr Alexander Mazur, and Dr Chirag M. Sandesara, previous contributors to this topic.
Declarações
GS, RMS, WL, AM, and CMS declare that they have no competing interests.
Revisores
Nora Goldschlager, MD
Professor of Clinical Medicine
University of California
Chief
Clinical Cardiology
San Francisco General Hospital
Director
Coronary Care Unit
ECG Laboratory and Pacemaker Clinic
San Francisco
CA
Declarações
NG declares that she has no competing interests.
Paul Heidenreich, MD
Associate Professor of Medicine
Stanford University
Stanford
CA
Declarações
PH declares that he has no competing interests.
Juan M. Sztajzel, MD
Cardiology Center and Medical Polyclinics
University Hospital Geneva
Geneva
Switzerland
Declarações
JMS declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Mangrum JM, DiMarco JP. The evaluation and management of bradycardia. N Engl J Med. 2000 Mar 9;342(10):703-9. Resumo
Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Aug 20;74(7):e51-156.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Bigeminismo ventricular
- Contrações ventriculares prematuras frequentes
- Fibrilação atrial
Mais Diagnósticos diferenciaisDiretrizes
- 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy
- 2020 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care
Mais DiretrizesFolhetos informativos para os pacientes
Bradicardia
Mais Folhetos informativos para os pacientesVideos
Como realizar uma demonstração animada do ECG
Mais vídeosConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal