小结
定义
病史和体格检查
关键诊断因素
- presença de fatores de risco
- edema no joelho
- sensação de instabilidade ou perda de apoio repentina/travamento do joelho
- dor no joelho
- sensibilidade e crepitação na interlinha articular
其他诊断因素
- cisto poplíteo (cisto de Baker) em casos crônicos
- amplitude de movimentos limitada
危险因素
- trauma agudo (lesão por torção)
- artrite do joelho
- instabilidade do joelho
- história de lesão do ligamento cruzado anterior
- desalinhamento da articulação do joelho
- superfície irregular ou desigual para prática esportiva
- condições de solo/meteorológicas desfavoráveis
- idade avançada
- trabalhos manuais e na construção civil
- menisco discoide
- índice de massa corporal (IMC) alto
诊断性检查
首要检查
- testes clínicos
- ressonância nuclear magnética (RNM)
- radiografia
需考虑的检查
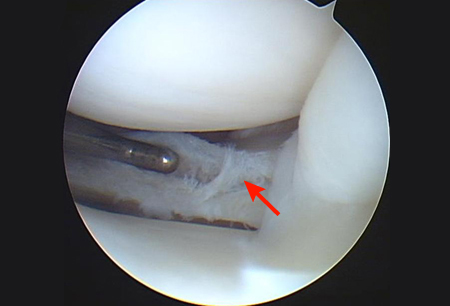
- artroscopia
- artrografia por tomografia computadorizada (TC)
- ultrassonografia
治疗流程
todos os pacientes
撰稿人
作者
Hideki Takeda, MD
Orthopedic Surgeon
Department of Sports Orthopedics
NTT Medical Center Tokyo
Tokyo
Japan
利益声明
HT declares that he has no competing interests.
鸣谢
Dr Hideki Takeda would like to gratefully acknowledge Dr Lars Engebretsen and Dr Kevin R. Stone, previous contributors to this topic.
利益声明
LE declares that he has no competing interests. KRS is an author of several references cited in this topic.
同行评议者
Daniel Solomon, MD
Co-Director of Orthopedic Sports and Shoulder Service
Department of Orthopedic Surgery
Naval Medical Center San Diego
San Diego
CA
利益声明
DS declares that he has no competing interests.
Jung-Ro Yoon, MD
Orthopedic Surgeon
Department of Orthopedic Surgery
Seoul Veterans Hospital
Seoul
South Korea
利益声明
JRY declares that she has no competing interests.
Nikunj N. Trivedi, MD
Fellow
Sports Medicine and Shoulder Surgery
Stanford University
Stanford
CA
利益声明
NNT declares that he has no competing interests.
Seth L. Sherman, MD
Associate Professor of Orthopedic Surgery
Fellowship Director
Sports Medicine and Shoulder Surgery
Stanford University
Stanford
CA
利益声明
SLS declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
参考文献
关键文献
Kopf S, Beaufils P, Hirschmann MT, et al. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2020 Apr;28(4):1177-94.全文 摘要
American Physical Therapy Association. Knee pain and mobility impairments: meniscal and articular cartilage lesions, revision 2018. 2018 [internet publication].
American College of Radiology. ACR Appropriateness Criteria® acute trauma to the knee. 2019 [internet publication].全文
参考文献
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
鉴别诊断
- Ruptura do ligamento cruzado anterior
- Entorse do ligamento colateral medial
- Entorse do ligamento cruzado posterior
更多 鉴别诊断指南
- Acute isolated meniscal pathology
- Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus
更多 指南患者教育信息
Osteoartrose: o que é?
更多 患者教育信息登录或订阅即可浏览 BMJ Best Practice 临床实践完整内容
内容使用需遵循免责声明