Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- perda de peso
- retardo do crescimento pôndero-estatural
- vômitos
- hipotensão
- genitália atípica
- hiperpigmentação
Outros fatores diagnósticos
- baixa estatura
- puberdade precoce
- menstruação irregular
- infertilidade
- calvície de padrão masculino (mulheres)
- ovários policísticos
- hirsutismo
- acne
Fatores de risco
- predisposição genética
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- 17-hidroxiprogesterona (17-OHP) sérica
- teste de estímulo com o hormônio adrenocorticotrófico (ACTH)
- cortisol sérico
- bioquímica sérica
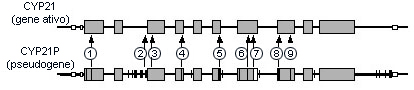
- análise genética
- cariótipo ou hibridização fluorescente in situ (FISH) para detecção dos cromossomos X e Y
Investigações a serem consideradas
- medição de esteroides adicionais
- mensuração da renina plasmática/atividade da renina plasmática
- ultrassonografia adrenal e pélvica
Algoritmo de tratamento
durante cirurgia, afecção febril ou outros estresses
HAC na forma clássica
forma não clássica
Colaboradores
Autores
Maria Vogiatzi, MD
Professor of Pediatrics
Division of Endocrinology and Diabetes
Children’s Hospital of Philadelphia
Philadelphia
PA
Declarações
MV is a consultant for Spruce Bioscience, Crinetics and Eton Pharmaceuticals and receives research support from Neurocrine Bioscience, Spruce Bioscience, Adrenas Therapeutics and Crinetics Pharmaceuticals lnc.
Marissa J Kilberg, MD, MSEd
Assistant Professor of Pediatrics
Division of Endocrinology and Diabetes
Children’s Hospital of Philadelphia
Philadelphia
PA
Declarações
MK has received consulting fees from Verily, Inc. related to type 1 diabetes. MK receives salary and travel support from the Cystic Fibrosis Foundation as part of the EnVisionIII cohort. MK participates in industry sponsored research but is not the direct recipient of these grants and receives no salary support or travel support from this.
Agradecimentos
The contributors would like to gratefully acknowledge Dr Mabel Yau, Dr Ahmed Kattab, Dr Saroj Nimkarn, Dr Karen Lin-Su, Dr Oksana Lekarev, Dr Maria New, Dr Jessica Kaltman and Dr Adnan Qamar, previous contributors to this topic. MY, AK, SN, JK and AQ declare that they no competing interests. KLS is medical director of the CARES Foundation and an author of several references cited in this topic. OL is on the Medical Advisory Board of the CARES Foundation. MN is an author of several references cited in this topic.
Revisores
Richard Auchus, MD, PhD
Professor of Internal Medicine
Division of Metabolism, Endocrinology and Diabetes
University of Michigan
Ann Arbor
MI
Declarações
RA contributed to the Endocrine Society CPG on CAH and has been on the board of directors for the past 3 years. He has conducted CAH-related contracted clinical trials and has consulted for Janssen Pharmaceuticals, Millendo Therapeutics, Spruce Biosciences, Neurocrine Biosciences, and Diurnal Ltd.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
White PC, Speiser PW. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr Rev. 2000 Jun;21:245-91.Texto completo Resumo
Merke DP, Auchus RJ. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. N Engl J Med. 2020 Sep 24;383(13):1248-61. Resumo
Claahsen-van der Grinten HL, Speiser PW, Ahmed SF, et al. Congenital adrenal hyperplasia-current insights in pathophysiology, diagnostics, and management. Endocr Rev. 2022 Jan 12;43(1):91-159.Texto completo Resumo
Speiser PW, Arlt W, Auchus RJ, et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 Nov 1;103(11):4043-88.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- hipoplasia adrenal congênita (HAC) ligada ao cromossomo X
- Causas genéticas da insuficiência adrenal primária
- Doença de Addison
Mais Diagnósticos diferenciaisDiretrizes
- Guidelines on paediatric urology
- Best practice guidelines for molecular genetic testing and reporting of 21-hydroxylase deficiency
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal