Resumo
Definición
Anamnesis y examen
Principales factores de diagnóstico
- presença de fatores de risco
- a dor é exacerbada pela atividade
- local da dor na região anteromedial do joelho com o joelho fletido a 90°
- local da dor na região lateral do cotovelo
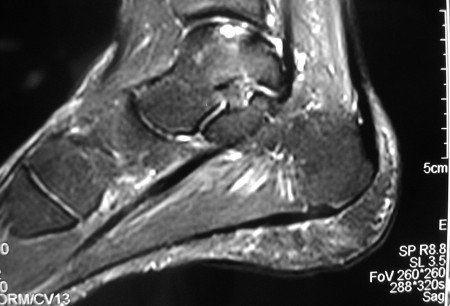
- local da dor na região posteromedial do tornozelo dorsifletido ou região anterolateral do tornozelo em flexão plantar
- presença de derrame
- bloqueio da articulação
- travamento da articulação
- amplitude de movimentos reduzida
Otros factores de diagnóstico
- comprometimento do joelho, idade de 10 a 20 anos
- comprometimento do cotovelo, idade entre 11 a 21 anos
- comprometimento do tálus, da segunda à quarta década
- ausência de história de trauma envolvendo o joelho ou cotovelo
- marcha antálgica na osteocondrite dissecante comprometendo o joelho ou tálus
- marcha de rotação externa na osteocondrite dissecante comprometendo o joelho
- fatores de alívio: anti-inflamatórios não esteroidais (AINEs), repouso, gelo, elevação
- crepitação
- teste de Wilson
- atrofia do quadríceps
Factores de riesgo
- estresse valgo/arremesso repetitivo
- ginástica/levantamento de peso nos membros superiores
- entorse/instabilidade do tornozelo
- atividades atléticas competitivas
- história familiar
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- radiografias do joelho
- radiografias do tornozelo
- radiografia panorâmica do membro inferior
- radiografias do cotovelo
Pruebas diagnósticas que deben considerarse
- tomografia computadorizada (TC)
- RNM
- Artrorressonância
- artroscopia diagnóstica
Algoritmo de tratamiento
joelho
cotovelo
tornozelo (tálus)
Colaboradores
Autores
Henry G. Chambers, MD
Professor of Clinical Orthopedic Surgery
University of California, San Diego
Rady Children’s Hospital
San Diego
CA
Divulgaciones
HGC is an author of a number of references cited in this topic.
Agradecimientos
Dr Henry G. Chambers would like to gratefully acknowledge Dr James L. Carey, Dr Jon Divine, Dr Michael Nett, and Dr Cedric Ortiguera, the previous contributors to this topic.
Divulgaciones
JLC is an author of a number of references cited in this topic. JD, MN, and CO declared that they had no competing interests.
Revisores por pares
James E. McGrory, MD
Orthopedic Surgeon
The Hughston Clinic PC
Columbus
GA
Divulgaciones
JEM declares that he has no competing interests.
Nicola Maffulli, MD, MS, PhD, FRCS(Orth)
Centre Lead and Professor of Sports and Exercise Medicine
Consultant Trauma and Orthopaedic Surgeon
Barts and The London School of Medicine and Dentistry
Institute for Health Sciences Education
Centre for Sports and Exercise Medicine
Queen Mary University of London
Mile End Hospital
London
UK
Divulgaciones
NM declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Kocher MS, Tucker R, Ganley TJ, et al. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006 Jul;34(7):1181-91. Resumen
American Academy of Orthopaedic Surgeons. Diagnosis and treatment of osteochondritis dissecans. Dec 2023 [internet publication].Texto completo
Perumal V, Wall E, Babekir N. Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop. 2007 Oct-Nov;27(7):821-5. Resumen
Baker CL 3rd, Baker CL Jr, Romeo AA. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010 Sep;38(9):1917-28. Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Fratura osteocondral
- Ruptura do menisco
- Artrite séptica
Más DiferencialesGuías de práctica clínica
- Osteochondritis dissecans: diagnosis and treatment
Más Guías de práctica clínicaInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad