Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
- corona flebectática (exacerbação maleolar ou exacerbação do tornozelo)
- edema maleolar
- hiperpigmentação (edema acastanhado)
- lipodermatoesclerose
- atrofia branca
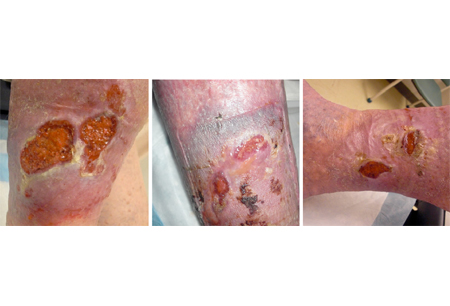
- úlceras da perna
Outros fatores diagnósticos
- fadiga, dor e/ou desconforto nas pernas
- sensação de peso nas pernas
- cãibras nas pernas
- telangiectasias
- veias reticulares
- veias tortuosas dilatadas
- pele ressecada e escamosa
- queimadura e prurido na pele
- edema unilateral de membro inferior
Fatores de risco
- idade mais avançada
- história familiar
- tabagismo
- trombose venosa profunda
- profissão ortostática
- sexo feminino
- obesidade (circunferência da cintura)
- frouxidão ligamentar
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- ultrassonografia duplex
Investigações a serem consideradas
- flebografia ascendente
- venografia por tomografia computadorizada (TC)
- venografia por ressonância magnética
- TC abdominal e de pelve
- ultrassonografia do abdome e da pelve
- ultrassonografia intravascular
- pletismografia a ar
Algoritmo de tratamento
todos os pacientes sintomáticos
Colaboradores
Autores
Joseph L. Mills Sr, MD
Professor and Chief
Division of Vascular Surgery and Endovascular Therapy
Michael E. DeBakey Department of Surgery
Baylor College of Medicine
Houston
TX
Declarações
JLM declares that he has no competing interests.
David G. Armstrong, DPM, MD, PhD
Professor of Surgery
Director of Southwestern Academic Limb Salvage Alliance (SALSA)
Keck School of Medicine of University of Southern California (USC)
Los Angeles
CA
Declarações
DGA declares that his work is partially supported by grants from the National Institutes of Health and the National Institute of Diabetes and Digestive and Kidney Diseases.
Revisores
Anahita Dua, MD, MS, MBA, FACS
Assistant Professor of Surgery
Massachusetts General Hospital/Harvard Medical School
Boston
MA
Declarações
AD declares that she has no competing interests.
Paul Tisi, MBBS, MS, FRCSEd
Medical Director/Consultant Vascular Surgeon
Bedford Hospital
Bedford
UK
Declarações
PT declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Lurie F, Passman M, Meisner M, et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. 2020 May;8(3):342-52. Resumo
De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor's choice - European Society for Vascular Surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg. 2022 Feb;63(2):184-267.Texto completo Resumo
Bergan JJ, Schmid-Schönbein GW, Smith PD, et al. Chronic venous disease. N Engl J Med. 2006 Aug 3;355(5):488-98. Resumo
American Vein and Lymphatic Society (American College of Phlebology). Treatment of superficial venous disease of the lower leg. Feb 2016 [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Úlcera do pé diabético
- Úlcera arterial
- Carcinoma de células escamosas (Marjolin)
Mais Diagnósticos diferenciaisDiretrizes
- ACR-AIUM-SPR-SRU practice parameter for the performance of peripheral venous ultrasound examination
- ACR appropriateness criteria® lower extremity chronic venous disease
Mais DiretrizesFolhetos informativos para os pacientes
Diabetes do tipo 2: devo tomar insulina?
Insuficiência cardíaca: como posso me ajudar?
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal