Summary
Definition
History and exam
Key diagnostic factors
- diarreia, especialmente diarreia hemorrágica
- infância, especialmente <5 anos de idade
Other diagnostic factors
- surto na comunidade conhecido de E coli produtora da toxina Shiga
- história de ingestão de alimentos que podem ter sido contaminados com E coli produtor da toxina Shiga
- efeito adverso incomum após o tratamento com ciclosporina, alguns agentes quimioterápicos, agentes direcionados ao câncer e quinina
- estado de gravidez ou pós-parto
- efeito adverso incomum após transplante de medula óssea
- história familiar de possível síndrome tipo síndrome hemolítico-urêmica (SHU)
Risk factors
- ingestão de alimentos ou de água contaminada
- surto na comunidade conhecido de E coli toxogênica
- exposição a indivíduos infectados em ambientes institucionais
- predisposição genética (SHU atípica)
- transplante de medula óssea
- exposição à ciclosporina, alguns agentes quimioterápicos, agentes específicos para câncer e quinina
- relacionada à gravidez ou ao pós-parto
Diagnostic investigations
1st investigations to order
- Hemograma completo
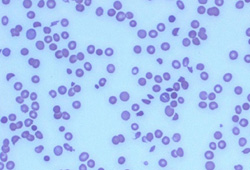
- esfregaço de sangue periférico
- função renal/creatinina
- eletrólitos séricos (sódio, potássio, cloreto e bicarbonato, cálcio e fósforo)
- tempo de protrombina (TP), TTP
- lactato desidrogenase (LDH)
- haptoglobina
- coprocultura em ágar MacConkey-sorbitol para detectar Escherichia coli produtora de toxina Shiga
- reação em cadeia da polimerase para detectar toxina Shiga 1/toxina Shiga 2
- proteínas envolvidas na regulação do complemento
Investigations to consider
- urinálise
- nível de ADAMTS13
- TFHs
- amilase sérica, lipase, glicose
Treatment algorithm
SHU associada a Escherichia coli produtora de toxina Shiga (STEC)
SHU atípica
SHU secundária: não devida a Streptococcus pneumoniae
SHU secundária: decorrente de S pneumoniae
Contributors
Authors
Sharon Andreoli, MD
Byron P. and Francis D. Hollet Professor of Pediatrics, Pediatric Nephrology
Indiana University School of Medicine
Indianapolis
IN
Disclosures
SA owns stock in Merck and Pfizer, and has been a consultant for Reata Pharmaceuticals. SA is on the Editorial Board of Pediatric Nephrology and the Journal of Pediatrics.
Myda Khalid, MD
Associate Professor of Pediatric Nephrology
Indiana University School of Medicine
Indianapolis
IN
Disclosures
MK declares that she has no competing interests.
Acknowledgements
Dr Sharon Andreoli and Dr Myda Khalid would like to gratefully acknowledge Dr Ann Zimrin and Dr John Hess, previous contributors to this topic.
Disclosures
AZ and JH declare that they have no competing interests.
Peer reviewers
Rebecca Connor, MD
Chief Fellow
Section of Hematology and Oncology
Department of Internal Medicine
Wake Forest University Baptist Medical Center
Winston-Salem
NC
Disclosures
RC declares that she has no competing interests.
References
Key articles
Fakhouri F, Zuber J, Frémeaux-Bacchi V, et al. Haemolytic uraemic syndrome. Lancet. 2017 Aug 12;390(10095):681-96. Abstract
Banatvala N, Griffin PM, Greene KD, et al. The United States national prospective hemolytic uremic syndrome study: microbiologic, serologic, clinical and epidemiologic findings. J Infect Dis. 2001 Apr 1;183(7):1063-70. Abstract
Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005 Mar 19-25;365(9464):1073-86. Abstract
Wong CS, Jelacic S, Habeeb RL, et al. The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000 Jun 29;342(26):1930-6.Full text Abstract
McKee RS, Schnadower D, Tarr PI, et al; Pediatric Emergency Medicine Collaborative Research Committee and Pediatric Emergency Research Canada. Predicting hemolytic uremic syndrome and renal replacement therapy in Shiga toxin-producing Escherichia coli-infected children. Clin Infect Dis. 2020 Apr 10;70(8):1643-51.Full text Abstract
Boyce TG, Swerdlow DL, Griffin PM. Escherichia coli O157:H7 and the hemolytic uremic syndrome. N Engl J Med. 1995 Aug 10;333(6):364-8. Abstract
Rathbone J, Kaltenthaler E, Richards A, et al. A systematic review of eculizumab for atypical haemolytic uraemic syndrome (aHUS). BMJ Open. 2013 Nov 4;3(11):e003573.Full text Abstract
Loirat C, Fakhouri F, Ariceta G, et al. An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016 Jan;31(1):15-39. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Púrpura trombocitopênica trombótica (PTT)
- Hipertensão maligna
- Lúpus eritematoso sistêmico (LES)
More DifferentialsGuidelines
- Guidelines on hemolytic uremic syndrome by Indian Society of Pediatric Nephrology: key messages
- Hemolytic uremic syndrome in a developing country: consensus guidelines
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer