Resumen
Definición
Anamnesis y examen
Principales factores de diagnóstico
- presença de fatores de risco
- peso corporal significativamente baixo
- medo de ganhar peso ou engordar ou comportamentos que interferem no ganho de peso, apesar das evidências de peso corporal significativamente baixo
- imagem corporal distorcida
- restrição calórica
- compulsão alimentar periódica e/ou purgativa
- uso indevido de laxantes, diuréticos ou comprimidos dietéticos
- amenorreia
- diminuição da gordura subcutânea
Otros factores de diagnóstico
- fadiga geral, fraqueza muscular e baixa concentração
- significativa preocupação com pensamentos sobre comida
- hipotensão ortostática
- sintomas gastrointestinais inespecíficos
- sinais e sintomas cardíacos
- alterações nos cabelos, pele e unhas
- edema dependente
- osteopenia ou osteoporose
Factores de riesgo
- sexo feminino
- adolescência e puberdade
- traços obsessivos e perfeccionistas
- exposição à mídia ocidental
- influência genética
- classes socioeconômicas média e alta
- atleta
- provocações relacionadas à aparência
- maus-tratos na infância
- doença celíaca
- diabetes mellitus do tipo 1
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- diagnóstico clínico
- Hemograma completo
- bioquímica sérica
- testes da função tireoidiana
- testes da função hepática
- glicose sanguínea
- urinálise
- Teste de sentar, levantar e agachar
Pruebas diagnósticas que deben considerarse
- Questionário SCOFF (Enjoado [Sick], Controle [Controle], Uma medida [One stone], Gordo [Fat], Comida [Food])
- eletrocardiograma (ECG)
- densitometria óssea (absorciometria por dupla emissão de raios X)
- estradiol em indivíduos do sexo feminino
- testosterona em indivíduos do sexo masculino
- teste de gravidez urinário ou sérico
Algoritmo de tratamiento
clinicamente estável e adequado para tratamento ambulatorial
medicamente instável ou falha no tratamento ambulatorial
Colaboradores
Authors
Evelyn Attia, MD
Professor of Psychiatry
Columbia University and Weill Cornell Medical College
New York
NY
Disclosures
EA receives royalties from UpToDate and Oxford University Press for authorship and has served as a clinical advisor to Equip Health, Inc.
B. Timothy Walsh, MD
Professor of Psychiatry
Columbia University
New York
NY
Disclosures
BTW has received royalties and honoraria for writing, editing, speaking, or consulting from Guilford Publications, McGraw-Hill, Oxford University Press, UpToDate, Wiley, the University of British Columbia, Silverhill Hospital, the University of Alabama, the American Society for Clinical Psychopharmacology, Health Advances, and Dell Medical School.
Acknowledgements
Professor Evelyn Attia and Professor B. Timothy Walsh would like to gratefully acknowledge Dr Pauline S. Powers and Dr Abby M. Irwin, previous contributors to this topic.
Disclosures
PSP and AMI declare that they have no competing interests.
Peer reviewers
Heather Thompson-Brenner, MD
Director
Eating Disorders Program Center for Anxiety and Related Disorders
Psychology Department
Boston University
Boston
MA
Divulgaciones
HTB declares that she has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed., text revision (DSM-5-TR). Washington, DC: American Psychiatric Publishing; 2022.
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment. Dec 2020 [internet publication].Texto completo
American Psychiatric Association. Practice guideline for the treatment of patients with eating disorders. Feb 2023 [internet publication].Texto completo
Royal College of Psychiatrists. Medical emergencies in eating disorders (MEED): guidance on recognition and management. Oct 2023 [internet publication].Texto completo
Hornberger LL, Lane MA, Committee on Adolescence. Identification and management of eating disorders in children and adolescents. Pediatrics. 2021 Jan;147(1):e2020040279.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Bulimia nervosa
- Transtorno da evitação/restrição de ingestão alimentar
- Depression
Más DiferencialesGuías de práctica clínica
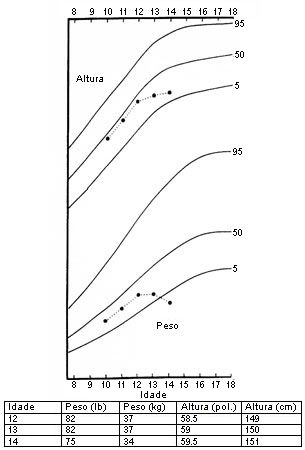
- Determining treatment goal weights for children and adolescents with anorexia nervosa
- Practice guideline for the treatment of patients with eating disorders
Más Guías de práctica clínicaFolletos para el paciente
Anorexia: perguntas a fazer ao seu médico
Anorexia
Más Folletos para el pacienteCalculadoras
Percentis do índice de massa corporal (IMC) para meninos (2 a 20 anos)
Percentis do índice de massa corporal (IMC) para meninas (2 a 20 anos)
Más CalculadorasInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad