Resumen
Definición
Anamnesis y examen
Principales factores de diagnóstico
- presença de fatores de risco
- dor abdominal
- diarreia prolongada
- lesões perianais
Otros factores de diagnóstico
- obstrução intestinal
- sangue nas fezes
- fadiga
- desconforto abdominal
- perda de peso
- febre
- lesões orais
- massa abdominal
- manifestações extraintestinais (por exemplo, eritema nodoso ou pioderma gangrenoso)
Factores de riesgo
- etnia branca
- Ascendência judaica asquenaze
- idade de 15-40 ou 50-60 anos
- história familiar de DC
- uso de antibióticos
- tabagismo
- dieta com alto teor de açúcar refinado
- dieta com baixo teor de fibras
- dieta com alto teor de alimentos ultraprocessados
- uso de pílula contraceptiva oral
- não amamentados
- uso de anti-inflamatórios não esteroidais (AINEs)
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- Hemograma completo
- perfil de ferro (ferro sérico, ferritina sérica, capacidade total de ligação do ferro [TIBC], saturação da transferrina)
- vitamina B12 sérica
- folato sérico
- perfil metabólico completo (CMP)
- Proteína C-reativa e velocidade de hemossedimentação (VHS)
- exame de fezes
- sorologia para Yersinia enterocolitica
- radiografia abdominal simples
- RNM de abdome/pelve
- tomografia computadorizada (TC) abdominal
Pruebas diagnósticas que deben considerarse
- ultrassonografia abdominal e pélvica
- ileocolonoscopia
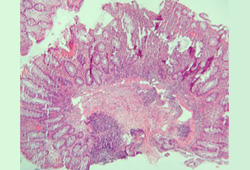
- biópsia tecidual
- endoscopia digestiva alta
- endoscopia por cápsula sem fio
- calprotectina fecal
Pruebas emergentes
- marcadores sorológicos:
Algoritmo de tratamiento
doença ileocecal não fistulizante com <100 cm do intestino afetado: apresentação inicial ou recidiva
doença colônica não fistulizante: apresentação inicial ou recidiva
doença do intestino delgado extensa (>100 cm do intestino afetado) não fistulizante: apresentação inicial ou recidiva
doença do trato gastrointestinal superior (doença esofágica e/ou gastroduodenal) não fistulizante: apresentação inicial ou recidiva
doença perianal ou fistulizante: apresentação inicial ou recidiva
em remissão
Colaboradores
Autores
Lucy Charlotte Hicks, MBBS, PhD, FHEA, MRCP
Consultant Gastroenterologist
Department of Gastroenterology
St Mary's Hospital
Imperial College Healthcare NHS Trust
Honorary Senior Clinical Lecturer
Imperial College
London
UK
Divulgaciones
LCH has received costs for travel and accommodation from Takeda.
Georgia Woodfield, MBChB, MSc, PhD, MRCP
Consultant Gastroenterologist
Department of Gastroenterology
Royal Free Hospital
Royal Free London NHS Foundation Trust
London
UK
Divulgaciones
GW declares that she has no competing interests.
Agradecimientos
Dr Georgia Woodfield and Dr Lucy Charlotte Hicks would like to gratefully acknowledge Mr George Reese, Dr Pranav H. Patel, Dr Philip J. Smith, Dr Charlotte Ford, Dr Wissam Bleibel, Dr Bishal Mainali, Dr Chandrashekhar Thukral, and Dr Mark A. Peppercorn, the previous contributors to this topic.
Divulgaciones
GR is an author of a number of references cited in this topic. PHP, PJS, CF, WB, BM, CT, and MAP declare that they have no competing interests.
Revisores por pares
Kiron M. Das, MD, PhD, FACP, FRCP
Chief of Gastroenterology & Hepatology
Professor of Medicine
Director of Crohn's & Colitis Center of New Jersey
New Brunswick
NJ
Divulgaciones
KMD declares that he has no competing interests.
John Mansfield, MA, MD, FRCP
Consultant Gastroenterologist and Senior Lecturer
Royal Victoria Infirmary
Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University
Newcastle upon Tyne
UK
Divulgaciones
JM declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific consensus statements on Crohn's disease. Part 1: definition, diagnosis, and epidemiology. J Gastroenterol Hepatol. 2016 Jan;31(1):45-55.Texto completo Resumen
Lichtenstein GR, Loftus EV, Isaacs KL, et al. ACG clinical guideline: management of Crohn's disease in adults. Am J Gastroenterol. 2018 Apr;113(4):481-517.Texto completo Resumen
Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn's disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017 Jan;11(1):3-25.Texto completo Resumen
Torres J, Bonovas S, Doherty G, et al. ECCO guidelines on therapeutics in Crohn's disease: medical treatment. J Crohns Colitis. 2020 Jan 1;14(1):4-22.Texto completo Resumen
Adamina M, Bonovas S, Raine T, et al. ECCO guidelines on therapeutics in Crohn's disease: surgical treatment. J Crohns Colitis. 2020 Feb 10;14(2):155-68.Texto completo Resumen
Feuerstein JD, Ho EY, Shmidt E, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021 Jun;160(7):2496-508.Texto completo Resumen
Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: surgical management and special situations. J Crohns Colitis. 2017 Feb;11(2):135-49.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Colite ulcerativa
- Colite infecciosa
- Colite pseudomembranosa
Más DiferencialesGuías de práctica clínica
- BSG consensus guidelines on the management of inflammatory bowel disease in adults
- Management of Crohn's disease in adults
Más Guías de práctica clínicaFolletos para el paciente
Doença de Crohn: quais são as opções de tratamento?
Doença de Crohn: o que é?
Más Folletos para el pacienteInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad