Summary
Definition
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
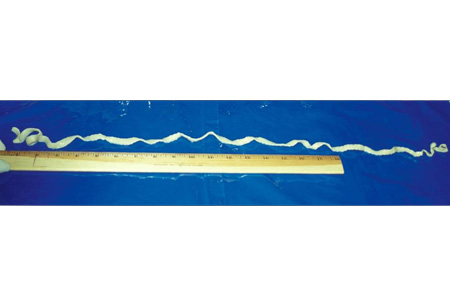
- segmentos do verme nas fezes
- pressão intracraniana elevada
- convulsões
- hepatomegalia
- tosse
- hemoptise
- manifestações alérgicas
- anemia
Outros fatores diagnósticos
- assintomático
- sintomas intestinais vagos
- perturbação do sono
- cefaleias
- erupção cutânea
- nódulos subcutâneos
- pirexia
- distúrbios visuais
Fatores de risco
- morar em fazendas
- higiene precária
- consumir ou manusear carne malcozida
- consumir ou manusear peixe ou crustáceos malcozidos
- ingestão de água contaminada
- proprietários de cães
- atividades ao ar livre
- idade <12 anos
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- exame de fezes
- hemograma completo
- ensaio EITB (Enzime-Linked Immunoelectrotransfer Blot Assay)
- Ensaio de imunoadsorção enzimática (ELISA) e sorologia Western Blot para equinococose
- ultrassonografia
- TC cranioencefálica
- RNM cranioencefálica/da coluna
Investigações a serem consideradas
- rastreamento de tuberculose e estrongiloidíase
Algoritmo de tratamento
doença do sistema nervoso central: com hipertensão intracraniana
doença intestinal
doença do sistema nervoso central: sem hipertensão intracraniana
doença hepática ou torácica
Colaboradores
Autores
Jose A. Serpa, MD, MS, CTropMed
Professor of Medicine
Section of Infectious Diseases
Baylor College of Medicine
Houston
TX
Declarações
JAS declares that he has no competing interests.
Agradecimentos
Dr Jose A. Serpa would like to gratefully acknowledge Dr Andrew Chou, Dr Christina Coyle, and Dr Maheen Saeed, previous contributors to this topic.
Declarações
AC and MS declare that they have no competing interests. CC is an author of several references cited in this topic.
Revisores
William A. Petri, Jr, MD, PhD, FACP
Chief and Professor of Medicine
Division of Infectious Diseases and International Health
University of Virginia Health System
Charlottesville
VA
Disclosures
WAP declares that he has no competing interests.
Linda Kalilani, MBBS, MPhil, PhD
Epidemiologist
College of Medicine
University of Malawi
Zomba
Malawi
Disclosures
LK declares that she has no competing interests.
Paul Roberts, MD
Assistant Professor
Family Medicine
Mayo Clinic
Jacksonville
FL
Disclosures
PR declares that he has no competing interests.
References
Key articles
White AC Jr, Coyle CM, Rajshekhar V, et al. Diagnosis and treatment of neurocysticercosis: 2017 clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2018 Apr 3;66(8):e49-75.Full text Abstract
World Health Organization. WHO guidelines on management of Taenia solium neurocysticercosis. Sep 2021 [internet publication].Full text
Del Brutto OH, Nash TE, White AC Jr, et al. Revised diagnostic criteria for neurocysticercosis. J Neurol Sci. 2017 Jan 15;372:202-10.Full text Abstract
Centers for Disease Control and Prevention. Parasites - taeniasis: resources for health professionals. Oct 2020 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Tuberculoma do sistema nervoso central
- Abscesso amebiano
- Enxaqueca
More DifferentialsGuidelines
- CDC Yellow Book: health information for international travel - taeniasis
- CDC Yellow Book: health information for international travel - cysticercosis
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer