Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
- miose
- bradipneia
- estado mental alterado
- resposta dramática à naloxona
Outros fatores diagnósticos
- marcas de agulha recentes
- objetos próximos associados ao uso de drogas
- redução da motilidade gastrointestinal
- marcas de agulha antigas nos braços ou nas pernas
- estertores pulmonares
- escarro róseo e espumoso
- convulsões
- disritmias
Fatores de risco
- história de opioides prescritos
- transtorno e dependência relacionados ao uso de opioides
- abstinência recente em usuários crônicos
- tomar opioides por injeção
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- tentativa terapêutica com naloxona
- eletrocardiograma (ECG)
Investigações a serem consideradas
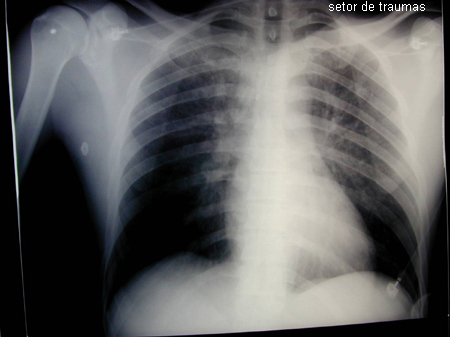
- radiografia torácica
- tomografia computadorizada (TC) abdominal
- radiografia abdominal
- triagem de opioides na urina
- cromatografia gasosa acoplada à espectrometria de massa
Algoritmo de tratamento
sem pacotes de substância retidos
com pacotes de substância retidos
Colaboradores
Autores
Ruben Thanacoody, MD, FRCP, FRCP(Edin), FEAPCCT
Consultant Physician and Clinical Toxicologist
Director, National Poisons Information Service (Newcastle)
Honorary Clinical Senior Lecturer, Newcastle University
Newcastle-upon-Tyne
UK
Declarações
RT declares that he has contributed to the Royal College of Emergency Medicine best practice guidelines on management of opioid toxicity in emergency departments and delivered a lecture at the RCEM Annual Conference in Gateshead. He has not received any payment for this work.
Agradecimentos
Dr Ruben Thanacoody would like to gratefully acknowledge Dr Dean Olsen, a previous contributor to this topic.
Declarações
DO declares that he has no competing interests.
Revisores
Joseph Donroe, null
Associate Professor of Medicine
Yale School of Medicine
New Haven
CO
Declarações
JD declares that he has no competing interests.
Anne-Maree Kelley, MD, MClinEd, FACEM
Director
Joseph Epstein Centre for Emergency Medicine Research
Western Health Sunshine Hospital
St Albans
Australia
Declarações
AMK has received grant funding for research into intranasal delivery of naloxone in heroin overdose.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Dowell D, Ragan KR, Jones CM, et al. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. 2022 Nov 4;71(3):1-95.Texto completo Resumo
Dezfulian C, Orkin AM, Maron BA, et al. Opioid-associated out-of-hospital cardiac arrest: distinctive clinical features and implications for health care and public responses: a scientific statement from the American Heart Association. Circulation. 2021 Apr 20;143(16):e836-70.Texto completo Resumo
Resuscitation Council UK. 2021 resuscitation guidelines. 2021 [internet publication].Texto completo
Williams K, Lang ES, Panchal AR, et al. Evidence-based guidelines for EMS administration of naloxone. Prehosp Emerg Care. 2019 Nov-Dec;23(6):749-63.Texto completo Resumo
Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Superdosagem de gama-hidroxibutirato (GHB)/gama-butirolactona (GBL)
- Superdosagem de clonidina/imidazolinas
- Superdosagem de antipsicóticos
Mais Diagnósticos diferenciaisDiretrizes
- Joint RCEM and NPIS best practice guideline: assessment and management of acute opioid toxicity in adults in the emergency department
- 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal