Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
- doença cardíaca
Outros fatores diagnósticos
- medicações
- palpitações
- fadiga, fraqueza
- dor torácica
- dispneia, tosse
- náuseas e vômitos
- tontura, síncope
- estertores
- edema
Fatores de risco
- uso indevido de substâncias (ingestão/abstinência de bebidas alcoólicas, cocaína, anfetaminas)
- toxicidade por digoxina
- cirurgia cardíaca prévia para corrigir os defeitos cardíacos congênitos
- doença arterial coronariana
- exacerbação da doença pulmonar crônica
- teofilina
Investigações diagnósticas
Primeiras investigações a serem solicitadas
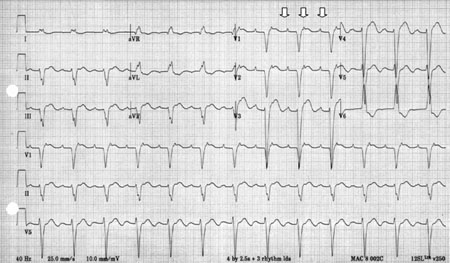
- eletrocardiograma (ECG)
- nível de digoxina
- nível de teofilina
- radiografia torácica
- eletrólitos
- análise toxicológica
Investigações a serem consideradas
- manobras vagais, adenosina
- hormônios estimulantes da tireoide
- ecocardiograma
- ECG ambulatorial de 24 horas (Holter) ou registro de eventos
- estudo eletrofisiológico (EF)
Algoritmo de tratamento
adultos: taquicardia supraventricular indiferenciada
adultos: taquicardia atrial focal; não há suspeita de excesso de digoxina
adultos: taquicardia atrial focal; suspeita de toxicidade por digoxina
criança
adultos: taquicardia atrial focal sustentada ou recorrente
Colaboradores
Autores
Danesh Kella, MBBS, FHRS
Assistant Professor
Department of Cardiovascular Diseases
Division of Heart Rhythm
Mayo Clinic
Jacksonville
FL
Declarações
DK receives honoraria from Zoll Medical.
Agradecimentos
Dr Danesh Kella would like to gratefully acknowledge Dr Sarah Stahmer, previous contributor to this topic.
Peer reviewers
Kathryn L. Berlacher, MD, MS
Assistant Professor and Cardiology Fellowship Program Director
University of Pittsburgh Medical Center
Pittsburgh
PA
Disclosures
KLB declares that she has no competing interests.
Mehak Dhande, MD
Clinical Cardiac Electrophysiology Fellow
University of Pittsburgh Medical Center
Pittsburgh
PA
Disclosures
MD declares that she has no competing interests.
Amal Mattu, MD
Associate Professor of Emergency Medicine
University of Maryland Medical Center
Baltimore
MD
Disclosures
AM declares that he has no competing interests.
Vias Markides, MB(Hons), BS(Hons), MD, FRCP
Consultant Cardiologist
Royal Brompton & Harefield NHS Trust
Imperial College London
London
UK
Disclosures
VM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115.Full text Abstract
Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020 Feb 1;41(5):655-720.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Taquicardia sinusal
- Taquicardia por reentrada no nó atrioventricular
- Taquicardia por reentrada AV ou taquicardia mediada por via acessória
More DifferentialsGuidelines
- JCS/JHRS 2020 guideline on pharmacotherapy of cardiac arrhythmias
- 2019 ESC guidelines for the management of patients with supraventricular tachycardia
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer