Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- hematêmese
Outros fatores diagnósticos
- vertigem/tontura
- hipotensão postural/ortostática
- disfagia
- odinofagia
- dor
- melena
- hematoquezia
- choque
- sinais de anemia
Fatores de risco
- afecções que predispõem ao esforço para vomitar, vômitos e/ou esforços
- tosse crônica
- hérnia hiatal
- esforço para vomitar durante endoscopia ou outra intervenção
- consumo significativo de bebidas alcoólicas
- instrumentação prévia
- idade entre 30 e 50 anos
- sexo masculino
- uso de aspirina ou outros anti-inflamatórios não esteroidais
- soluços
- trauma abdominal contuso
- ressuscitação cardiopulmonar
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- Hemograma completo
- ureia
- creatinina e eletrólitos
- testes da função hepática
- tempo de protrombina (TP)/razão normalizada internacional (INR)
- tempo de tromboplastina parcial (TTP)
- prova cruzada/tipagem sanguínea
- endoscopia digestiva alta (EDA) flexível
Investigações a serem consideradas
- tomografia computadorizada (TC) do tórax
- radiografia torácica
- angiografia
Algoritmo de tratamento
todos os pacientes
Colaboradores
Autores
Douglas G. Adler, MD, FACG, AGAF, FASGE
Professor of Medicine
Center Director
Center for Advanced Therapeutic Endoscopy (CATE)
Advent Health
Porter Adventist Hospital
Denver
CO
Declarações
DGA is a consultant for Merit Medical, Cook Endoscopy, Olympus America, and Boston Scientific.
Agradecimentos
Dr Douglas Adler would like to gratefully acknowledge Dr Shilpa Reddy and Dr Juan Carlos Munoz, the previous contributors to this topic.
Declarações
SR and JCM declare that they have no competing interests.
Revisores
Joseph Sung, MD
Professor of Medicine
Department of Medicine and Therapeutics
Director
Institute of Digestive Disease
The Chinese University of Hong Kong
Hong Kong
Declarações
JS declares that he has no competing interests.
Imtiyaz Mohammed, MD
Consultant Gastroenterologist
Sandwell General Hospital
Lyndon
West Bromwich
UK
Declarações
IM declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Alali AA, Barkun AN. An update on the management of non-variceal upper gastrointestinal bleeding. Gastroenterol Rep (Oxf). 2023 Mar 20;11:goad011.Texto completo Resumo
Laine L, Barkun AN, Saltzman JR, et al. ACG clinical guideline: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol. 2021 May 1;116(5):899-917.Texto completo Resumo
Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: guideline recommendations from the International Consensus Group. Ann Intern Med. 2019 Dec 3;171(11):805-22.Texto completo Resumo
American College of Radiology. ACR appropriateness criteria: nonvariceal upper gastrointestinal bleeding. 2024 [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Esofagite
- Perfuração espontânea do esôfago (síndrome de Boerhaave)
- Erosões de Cameron
Mais Diagnósticos diferenciaisDiretrizes
- ACR appropriateness criteria: nonvariceal upper gastrointestinal bleeding
- Management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period
Mais DiretrizesFolhetos informativos para os pacientes
Bulimia: perguntas a fazer ao seu médico
Úlceras pépticas
Mais Folhetos informativos para os pacientesCalculadoras
Escore de Blatchford para sangramento gastrointestinal
Escore de Rockall para hemorragia digestiva alta
Mais CalculadorasVideos
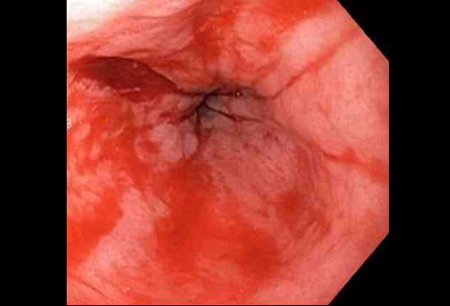
Laceração de Mallory-Weiss com sangramento
Laceração de Mallory-Weiss após cauterização com sonda bipolar
Mais vídeosConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal