Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presença de fatores de risco
- idade entre 10-19 ou 30-39 anos
- fraqueza motora
- parestesias ou perda sensorial
- sintomas vesicais: polaciúria, urgência, incontinência ou retenção urinária
- sintomas intestinais: incontinência ou constipação
- sinal de L'Hermitte
- Sinal de McArdle
- espasmos tônicos paroxísticos
- sinais do neurônio motor superior: hiper-reflexia, sinal de Babinski positivo, espasticidade dos membros
- perda sensorial/nível sensorial
- dispneia/dificuldade respiratória
Outros fatores diagnósticos
- dorsalgia
- dor no tronco/membros
- arreflexia/hiporreflexia
- soluços
- náuseas/vômitos
Fatores de risco
- doença infecciosa precedente
- vacinação recente
- sexo feminino
- história de trauma físico recente
- injeção na coluna vertebral
Investigações diagnósticas
Primeiras investigações a serem solicitadas
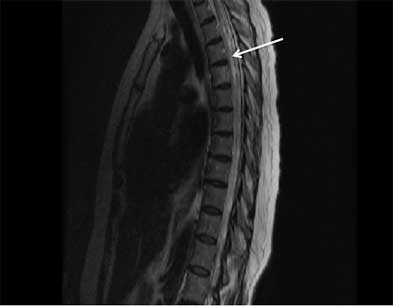
- ressonância nuclear magnética (RNM) da medula espinhal
- ressonância nuclear magnética (RNM) cranioencefálica
- autoanticorpos anti-aquaporina-4 e autoanticorpos anti-glicoproteína mielina-oligodendrócito séricos
- celularidade do líquido cefalorraquidiano, diferencial de celularidade, nível de proteínas, índice de imunoglobulina G (IgG) e bandas oligoclonais
- coloração de Gram, culturas (bacteriana, fúngica e para tuberculose) e esfregaço com tinta nanquim no líquido cefalorraquidiano
- líquido cefalorraquidiano, reação em cadeia da polimerase para detecção de vírus do herpes simples (HSV)-1, HSV-2, vírus da varicela-zóster (VZV), Borrelia burgdorferi (doença de Lyme), citomegalovírus (CMV), vírus Epstein-Barr (EBV) e vírus do Nilo Ocidental
- exame Venereal Disease Research Laboratory do líquido cefalorraquidiano
- fator antinuclear sérico, DNA de fita dupla
- antígeno nuclear extraível (incluindo autoanticorpos SSA e SSB)
- autoanticorpos paraneoplásicos séricos ou no líquido cefalorraquidiano
- outros autoanticorpos neurais
Investigações a serem consideradas
- enzima conversora de angiotensina sérica e do líquido cefalorraquidiano
- radiografia torácica
- tomografia computadorizada (TC) corporal (tórax, abdome e pelve)
- PET do corpo inteiro
- citometria de fluxo e citologia do líquido cefalorraquidiano
- sorologia para vírus do herpes simples (HSV) -1, HSV-2, vírus da varicela-zóster, citomegalovírus, vírus Epstein-Barr e vírus do Nilo Ocidental
- urinálise
- anticorpos antivírus da imunodeficiência humana (anti-HIV)
- potencial evocado visual
- tomografia de coerência óptica
- tentativa terapêutica com corticosteroide
- biópsia da medula espinhal
Algoritmo de tratamento
deficits neurológicos agudos
mielite transversa (MT) idiopática
com risco de esclerose múltipla (EM) (lesões desmielinizantes típicas na ressonância nuclear magnética [RNM])
soropositivo para autoanticorpos anti-aquaporina-4 (AQP4)
soropositivo para autoanticorpos IgG anti-glicoproteína mielina-oligodendrócito
Colaboradores
Autores
Cristina Valencia-Sanchez, MD, PhD
Department of Neurology
Mayo Clinic
Scottsdale
AZ
Declarações
CVS declares that she has served on an advisory board for TG Therapeutics.
Agradecimentos
Dr Cristina Valencia-Sanchez would like to gratefully acknowledge Dr Dean Wingerchuk, the previous contributor to this topic. DMW has received compensation from MedImmune for service on a clinical trial adjudication committee, from Caladrius for consulting services, and research support paid to Mayo Clinic from Alexion and TerumoBCT. DMW is an author of a number of references cited in this topic.
Revisores
Alireza Minagar, MD
Assistant Professor of Neurology
LSU Health Sciences Center
Shreveport
LA
Declarações
AM declares that he has no competing interests.
Cory Toth, BSc, MD, FRCP(C)
Assistant Professor of Neurosciences
Hotchkiss Brain Institute
University of Calgary
Alberta
Canada
Declarações
CT declares that he has no competing interests.
Abhijit Chaudhuri, DM, MD, PhD, FACP, FRCP
Consultant Neurologist
Clinical Director of Neurosciences
Department of Neurology
Queen's Hospital
Romford
UK
Declarações
AC declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002 Aug 27;59(4):499-505. Resumo
Expert Panel on Neurological Imaging, Agarwal V, Shah LM, et al. ACR appropriateness criteria® myelopathy: 2021 update. J Am Coll Radiol. 2021 May;18(5s):S73-82.Texto completo Resumo
Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis. Neurology. 2018 Apr 24;90(17):777-88.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Mielopatia compressiva
- Mielite infecciosa (por exemplo, tuberculose)
- Oclusão da artéria espinhal anterior
Mais Diagnósticos diferenciaisDiretrizes
- ACR appropriateness criteria: myelopathy
- Practice guideline: disease modifying therapies in adults with multiple sclerosis
Mais DiretrizesFolhetos informativos para os pacientes
Esclerose múltipla
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal