Summary
Definition
History and exam
Key diagnostic factors
- viral syndrome (prior)
- autoimmune disease
- infectious disease
- use of certain drugs and exposure to toxins
Other diagnostic factors
- age <50 years
- chest pain
- dyspnea
- orthopnea
- fatigue
- palpitations
- rales
- elevated neck veins
- S3 gallop
- sinus tachycardia
- atrial and ventricular arrhythmias
- tachypnea
- hepatomegaly
- syncope
- fever
- gastrointestinal issues
- rhinorrhea
- cough
- S3 and S4 summation gallop
- pericardial friction rub
- peripheral hypoperfusion
- hypotension
- altered sensorium
- lymphadenopathy
- respiratory distress
Risk factors
- infection (non-HIV)
- HIV infection
- autoimmune/immune-mediated diseases
- peripartum and postpartum periods
- use of certain drugs and exposure to toxins
- genetic variants
Diagnostic tests
1st tests to order
- 12-lead ECG
- CXR
- serum CK
- serum CK-MB
- serum troponin (I or T)
- serum B-type natriuretic peptide
- two-dimensional echocardiogram
Tests to consider
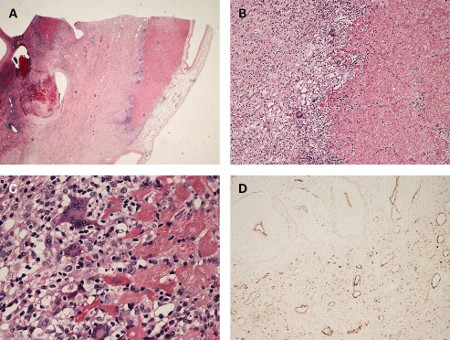
- endomyocardial biopsy (EMB)
- coronary angiography
- 18F-fluorodeoxyglucose positron emission tomography-computed tomography (FDG PET-CT)
- cardiac MRI
- viral polymerase chain reaction (PCR)
- genetic testing
Emerging tests
- MRI-guided EMB
Treatment algorithm
hemodynamically stable: no evidence of LV systolic dysfunction
hemodynamically stable: evidence of LV systolic dysfunction
hemodynamically unstable: adults
hemodynamically unstable: children
end-stage heart failure or refractory life-threatening arrhythmias
Contributors
Authors
Shriprasad R. Deshpande, MBBS, MS
Medical Director
Heart Transplant and Advanced Cardiac Therapies Program
Children's National Hospital
Associate Professor of Pediatrics
The George Washington University
Washington
DC
Disclosures
SRD declares that he has no competing interests.
Bibhuti Das, MBBS, MD, FAAP, FACC
Director of Heart Failure and Heart Transplant
Pediatric Cardiology
Methodist Children’s Hospital
San Antonio
TX
Disclosures
BD declares that he has no competing interests.
Acknowledgements
Dr Shriprasad R. Deshpande and Dr Bibhuti Das would like to gratefully acknowledge Dr Katherine C. Wu, Dr James E. Harvey, and Dr Arman T. Askari, previous contributors to this topic. KCW, JEH, and ATA declare that they have no competing interests.
Peer reviewers
David A. Leaf, MD, MPH
Professor of Medicine
School of Medicine
VA Greater Los Angeles Healthcare System
UCLA
Los Angeles
CA
გაფრთხილება:
DAL declares that he has no competing interests.
John Charpie, MD, PhD
Associate Professor of Pediatrics
Medical Director
Pediatric Cardiothoracic Intensive Care Unit
University of Michigan Congenital Heart Center
Ann Arbor
MI
გაფრთხილება:
JC declares that he has no competing interests.
Lokesh Tejwani, MD, FACC
Assistant Professor of Clinical Medicine
University of Missouri Hospitals and Clinics
Harry S. Truman VA Hospital
Columbia
MO
გაფრთხილება:
LT declares that he has no competing interests.
რეცენზენტების განცხადებები
BMJ Best Practice-ის თემების განახლება სხვადასხვა პერიოდულობით ხდება მტკიცებულებებისა და რეკომენდაციების განვითარების შესაბამისად. ქვემოთ ჩამოთვლილმა რეცენზენტებმა თემის არსებობის მანძილზე კონტენტს ერთხელ მაინც გადახედეს.
გაფრთხილება
რეცენზენტების აფილიაციები და გაფრთხილებები მოცემულია გადახედვის მომენტისთვის.
წყაროები
ძირითადი სტატიები
Lieberman EB, Hershkowitz A, Rose NR, et al. A clinicopathologic description of myocarditis. Clin Immunol Immunopathol. 1993 Aug;68(2):191-6. აბსტრაქტი
Law YM, Lal AK, Chen S, et al. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021 Aug 10;144(6):e123-35.სრული ტექსტი აბსტრაქტი
Writing Committee, Drazner MH, Bozkurt B, et al. 2024 ACC Expert Consensus Decision Pathway on strategies and criteria for the diagnosis and management of myocarditis: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2025 Feb 4;85(4):391-431.სრული ტექსტი აბსტრაქტი
Bozkurt B, Colvin M, Cook J, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016 Nov 3;134(23):e579-646.სრული ტექსტი აბსტრაქტი
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 May 3;145(18):e895-1032.სრული ტექსტი აბსტრაქტი
Aretz HT, Billingham ME, Edwards WD, et al. Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol. 1987 Jan;1(1):3-14. აბსტრაქტი
გამოყენებული სტატიები
ამ თემაში მოხსენიებული წყაროების სრული სია ხელმისაწვდომია მომხმარებლებისთვის, რომლებსაც აქვთ წვდომა BMJ Best Practice-ის ყველა ნაწილზე.
დიფერენციული დიაგნოზები
- Acute coronary syndrome
- Dilated cardiomyopathy
- Pericarditis
მეტი დიფერენციული დიაგნოზებიგაიდლაინები
- 2024 ACC Expert Consensus Decision Pathway on strategies and criteria for the diagnosis and management of myocarditis
- 2022 ESC Guidelines on cardio-oncology
მეტი გაიდლაინებიშედით სისტემაში ან გამოიწერეთ BMJ Best Practice
ამ მასალის გამოყენება ექვემდებარება ჩვენს განცხადებას