Summary
Definition
History and exam
Key diagnostic factors
- presencia de factores de riesgo
- anamnesis de traumatismos mecánicos
- historia clínica previa de osteoporosis o neoplasia
- dolor de espalda
- hematomas
- parestesia/entumecimiento agudo
- debilidad
- espasticidad muscular/clono (hipertonicidad) o hipotonía
- hiperreflexia o hiporreflexia
- signo de Hoffman
- signo de Babinski
- deformidad espinal
- pérdida del reflejo del esfínter anal
Other diagnostic factors
- ausencia del reflejo bulbocavernoso (S3-S4)
- signos de sección medular (hipotonía o flacidez que desaparecen dentro de las 24 horas)
- incontinencia urinaria
- retención urinaria indolora
Factores de riesgo
- caída desde una altura
- mecanismo de lesión de alta energía
- edad >65 años
- osteoporosis concomitante
- fractura vertebral previa
- lesión neoplásica subyacente
- trastornos inflamatorios o metabólicos subyacentes
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- TC multidetector sin contraste de la columna vertebral (TCMD)
Pruebas diagnósticas que deben considerarse
- radiografía de la columna toracolumbar (vistas anterior-posterior y lateral)
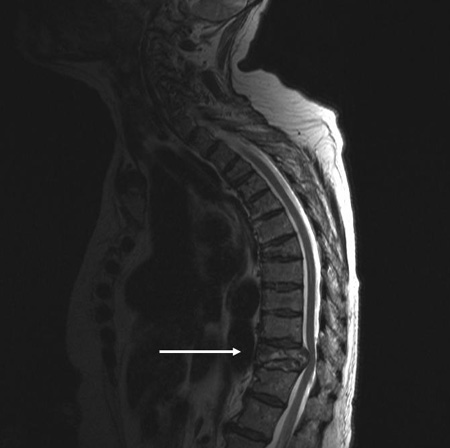
- imagen de resonancia magnética (IRM) de columna
- mielografía por TC
- IRM con secuencia STIR
- TC de cuerpo entero
Algoritmo de tratamiento
en la escena: lesiones en la columna vertebral posibles
fractura osteoporótica
fractura no osteoporótica
Colaboradores
Autores
Besnik Nurboja, BSc, MBBS, MD (Res), MRCS, FRCEM
Consultant in Emergency Medicine
Emergency Medicine
Epsom and St Helier University Hospital NHS Trust
London
UK
Divulgaciones
BN declares that he has no competing interests.
David Choi, FRCS(SN)

Consultant Neurosurgeon and Spinal Surgeon
The National Hospital for Neurology and Neurosurgery
London
UK
Divulgaciones
DC declares that he has no competing interests.
Revisores por pares
Byron F. Stephens, MD, MSCI
Associate Professor
Vanderbilt University School of Medicine
Nashville
TN
Divulgaciones
BFS has received Institutional Research Support from Nuvasive and Stryker.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Wendt K, Nau C, Jug M, et al. ESTES recommendation on thoracolumbar spine fractures: January 2023. Eur J Trauma Emerg Surg. 2024 Aug;50(4):1261-75.Texto completo
American College of Surgeons. Best practices guidelines. Spine injury. Mar 2022 [internet publication].Texto completo
American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].Texto completo
National Institute for Health and Care Excellence. Spinal injury: assessment and initial management. Feb 2016 [internet publication].Texto completo
O'Toole JE, Kaiser MG, Anderson PA, et al. Congress of Neurological Surgeons systematic review and evidence-based guidelines on the evaluation and treatment of patients with thoracolumbar spine trauma: executive summary. Neurosurgery. 2019 Jan 1;84(1):2-6.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Dolor musculoesquelético en la zona lumbar
- Traumatismo agudo de la columna cervical
- Enfermedad degenerativa de columna cervical
Más DiferencialesGuías de práctica clínica
- Clinical guidance for the effective identification of vertebral fractures
- Spinal injury: assessment and initial management
Más Guías de práctica clínicaFolletos para el paciente
Osteoporosis: ¿qué es?
Osteoartritis: ¿qué es?
Más Folletos para el pacienteCalculadoras
Escala de Coma de Glasgow
Más CalculadorasInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad