Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presencia de factores de riesgo
- amenorrea u oligomenorrea
- infertilidad
- galactorrea
- pérdida del deseo sexual (libido)
- disfunción eréctil
- deterioro visual (p. ej., hemianopsia temporal)
Outros fatores diagnósticos
- osteoporosis
- oftalmoplejía
- cefaleas
Fatores de risco
- predisposición genética (p. ej., presencia de una mutación que causa el síndrome de neoplasia endocrina múltiple tipo 1 [MEN-1] o adenoma hipofisario hereditario aislado [FIPA])
- terapia con estrógenos
- sexo masculino, de 30 a 60 años de edad
- sexo femenino, de 20 a 50 años de edad
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- prolactina sérica
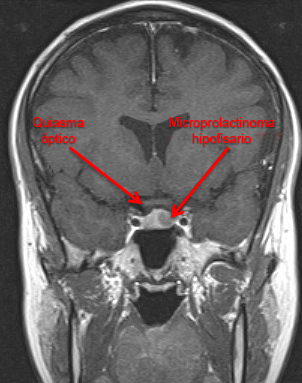
- resonancia magnética (IRM) hipofisaria
- examen computarizado del campo visual
Algoritmo de tratamento
mujeres en la etapa de la premenopausia
mujeres en la etapa de la posmenopausia
hombres
Colaboradores
Autores
Niamh Martin, MB ChB, PhD, FRCP
Reader in Endocrinology
Imperial Centre for Endocrinology
Department of Metabolism, Digestion and Reproduction
Imperial College London
London
UK
Declarações
NM declares that she has no competing interests.
Agradecimentos
Dr Niamh Martin would like to gratefully acknowledge Dr Ilan Shimon, the previous contributor to this topic.
Declarações
IS receives consultancy and lecturing fees from Pfizer, Israel, and is an author of a number of references cited in this topic.
Revisores
Mark Molitch, MD
Professor
Division of Endocrinology
Northwestern University Feinberg School of Medicine
Chicago
IL
Divulgaciones
MM is an author of a number of references cited in this topic.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Wildemberg LE, Fialho C, Gadelha MR. Prolactinomas. Presse Med. 2021 Dec;50(4):104080.Texto completo Resumen
Melmed S, Casanueva FF, Hoffman AR, et al; Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Feb;96(2):273-88.Texto completo Resumen
Xia MY, Lou XH, Lin SJ, et al. Optimal timing of dopamine agonist withdrawal in patients with hyperprolactinemia: a systematic review and meta-analysis. Endocrine. 2018 Jan;59(1):50-61. Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Macroadenomas hipofisarios no funcionales
- Hiperprolactinemia inducida por fármacos
- Hipotiroidismo primario
Más DiferencialesGuías de práctica clínica
- Position statement for clinical practice: prolactin-secreting tumors
- ACR appropriateness criteria: neuroendocrine imaging
Más Guías de práctica clínicaInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad
