Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- presencia de factores de riesgo
- sangrado vaginal anormal
- sangrado poscoital
- dolor pélvico o de espalda
- dispareunia
- masa en el cuello uterino
- sangrado en el cuello uterino
Outros fatores diagnósticos
- flujo vaginal mucoide o purulento
- obstrucción renal, intestinal o de vejiga
- dolor óseo
Fatores de risco
- infección por el virus del papiloma humano (VPH)
- grupo etario
- Infección por VIH
- inicio precoz de la actividad sexual (menores de 18 años)
- múltiples parejas sexuales
- tabaquismo
- inmunosupresión
- Exposición in útero al dietilestilbestrol
- antecedentes de enfermedades de transmisión sexual (ETS)
- uso de píldora anticonceptiva oral
- elevada cantidad de partos
- pareja masculina no circuncidada
- desnutrición por carencia de micronutrientes
- niveles bajos de folato sérico
- niveles bajos de vitaminas C y E
- consumo de alcohol
- bajo nivel socioeconómico
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- examen vaginal o con espéculo
- colposcopia
- biopsia
- pruebas del virus del papiloma humano (VPH)
Investigações a serem consideradas
- hemograma completo (HC)
- prueba de función renal
- pruebas de función hepática
- radiografía de tórax
- pielograma intravenoso
- ultrasonido renal
- enema de bario
- sigmoidoscopia
- cistoscopia
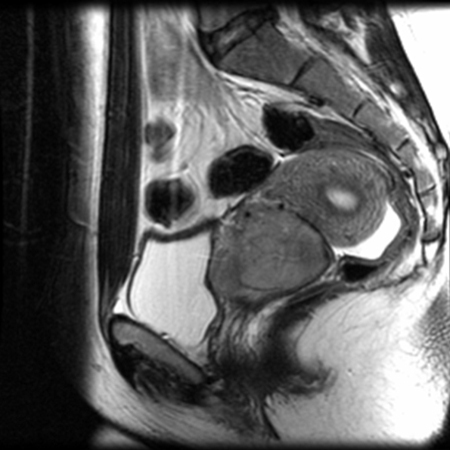
- resonancia magnética (IRM) de pelvis
- tomografía por emisión de positrones (TEP) de cuerpo entero
- tomografía por emisión de positrones/tomografía computarizada (TEP-TC) de cuerpo entero
- exploración por tomografía computarizada (TC) de tórax/ abdomen/pelvis con contraste por vía intravenosa y oral
- pruebas moleculares
Novos exames
- Expresión de biomarcadores p16 y Ki67
Algoritmo de tratamento
no embarazada en etapa IA1 sin LVSI: con deseo de fertilidad
no embarazada en etapa IA1 sin LVSI: sin deseo de fertilidad
no embarazada en etapa IA1 con LVSI: con deseo de fertilidad
no embarazada, etapa IA1 con LVSI: sin deseo de fertilidad
no embarazada, etapa IA2: con deseo de fertilidad
no embarazada, etapa IA2: sin deseo de fertilidad
no embarazada, etapa IB1: con deseo de fertilidad
no embarazada, etapa IB1: sin deseo de fertilidad
no embarazada, etapa IB2: con deseo de fertilidad
no embarazada, etapa IB2: sin deseo de fertilidad
no embarazada, etapa IA1:
no embarazada, etapa IB3 o IIA2
no embarazada, etapa IIB a IVA
no embarazada, etapa IVB (enfermedad metastásica)
no embarazada, enfermedad recurrente local o regional
embarazadas
Colaboradores
Autores
Richard T. Penson, MD, MRCP

Medical Gynecologic Oncologist
Division of Hematology Oncology
Massachusetts General Hospital
Boston
MA
Declarações
RTP reports serving on scientific advisory boards for Aadi Bioscience, AstraZeneca, GSK Inc., ImmunoGen Inc., Merck & Co., Roche Pharma, Sutro Biopharma, Tubulis GmbH; and serves on or chairs data and safety monitoring boards for AstraZeneca, EQRx, and Roche Pharma. RTP receives institutional research funding (as Principal Investigator) from 858 Therapeutics; royalties from BMJ Publishing, UptoDate, Elsevier Ltd, Wolters Kluwer Health, and Wiley-Blackwell; and payment for educational events from Research to Practice, ExpertConnect, ReachMD, and CMEO Outfitters.
Andrea L. Russo, MD
Director
Gynecologic Radiation Oncology
Associate Clinical Director
Department of Radiation Oncology
Massachusetts General Hospital
Boston
MA
Declarações
ALR declares that she has no competing interests.
Agradecimentos
Dr Richard T. Penson and Dr Andrea L. Russo would like to gratefully acknowledge Dr Larissa J. Lee, their co-contributor who is sadly deceased, and to acknowledge Dr Neil S. Horowitz and Dr Anthony H. Russell, previous contributors to this topic.
Declarações
NSH and AHR declare that they have no competing interests.
Revisores
Tracilyn Hall, MD
Assistant Professor of Gynecologic Oncology
Dan L Duncan Comprehensive Cancer Center
Baylor College of Medicine Houston
Houston
TX
Declarações
TH declares that she has no competing interests.
Linda Yang, MD
Fellow
Minimally Invasive Gynecologic Surgery
Magee Women's Hospital
University of Pittsburgh Medical Center
PA
Declarações
LY declares that she has no competing interests.
Deirdre Lyons, MB, BCh, BAO, MRCOG
Consultant in Obstetrics & Gynaecology
Lead Clinician in Colposcopy
Imperial College Healthcare NHS Trust
London
UK
Declarações
DL declares that she has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Marth C, Landoni F, Mahner S, et al. Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017 Jul 1;28(suppl 4):iv72-83.Texto completo Resumo
Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society CA Cancer J Clin. 2020 Sep;70(5):321-46.Texto completo Resumo
Bhatla N, Aoki D, Sharma DN, et al. Cancer of the cervix uteri: 2021 update. Int J Gynaecol Obstet. 2021 Oct;155 Suppl 1(suppl 1):28-44.Texto completo Resumo
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: cervical cancer [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Infección por el virus del papiloma humano (VPH)
- Infección pélvica
- Huevo de Naboth
Mais Diagnósticos diferenciaisDiretrizes
- Suspected cancer: recognition and referral
- Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV
Mais DiretrizesFolhetos informativos para os pacientes
Cáncer de cuello uterino
Vacuna contra el VPH (virus del papiloma humano)
Mais Folhetos informativos para os pacientesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer