Resumen
Definição
História e exame físico
Principais fatores diagnósticos
- presencia de factores de riesgo
- plétora facial
- plenitud supraclavicular
- estrías violáceas
- ausencia de embarazo
- irregularidades menstruales
- ausencia de desnutrición
- ausencia de alcoholismo
- ausencia de estrés fisiológico
- desaceleración del crecimiento lineal en niños
Outros fatores diagnósticos
- sexo femenino
- hipertensión
- intolerancia a la glucosa o diabetes mellitus
- osteoporosis prematura o fracturas inexplicables
- aumento de peso y obesidad central
- acné
- síntomas psiquiátricos
- libido disminuida
- tendencia a la formación de hematomas
- debilidad
- redondez facial
- almohadillas de grasa dorsocervicales
- nefrolitiasis inexplicable
- evento venotrombólico
- hirsutismo
Fatores de risco
- uso exógeno de corticosteroides
- adenoma hipofisario
- adenoma suprarrenal
- carcinoma suprarrenal
- tumores neuroendocrinos
- carcinoma torácico o broncogénico
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- prueba de embarazo en orina
- glucosa sérica
- cortisol salival nocturno
- prueba de supresión con dexametasona de 1 mg durante la noche
- cortisol libre urinario de 24 horas
- prueba de supresión con dexametasona de 2 mg (baja dosis) durante 48 horas
Investigações a serem consideradas
- cortisol sérico matutino y la hormona adrenocorticotropa (ACTH)
- nivel plasmático de sulfato de deshidroepiandrosterona (DHEAS)
- resonancia magnética (IRM) hipofisaria
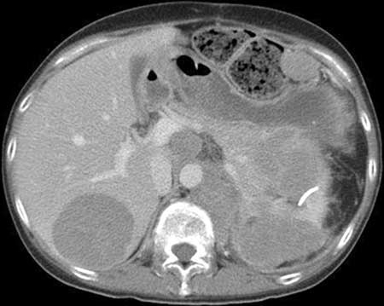
- estudios por imágenes suprarrenales
- prueba de supresión con dexametasona a dosis alta
- cateterismo de senos petrosos inferiores (CSPI)
- tomografía computarizada (TC) de tórax, abdomen y pelvis
- resonancia magnética (IRM) de tórax
- exploración con octreotida
- TEP/TC de galio-68 DOTATATE
Algoritmo de tratamento
Enfermedad de Cushing (tumor hipofisario secretor de hormona adrenocorticotropa [ACTH])
síndrome de hormona adrenocorticotrópica (ACTH) u hormona liberadora de corticotropina (CRH) ectópicas
independiente de la hormona adrenocorticotrópica (ACTH) provocado por carcinoma o adenoma suprarrenal unilateral
independiente de la hormona adrenocorticotrópica (ACTH) provocado por enfermedad suprarrenal bilateral (hiperplasia o adenoma)
secreción autónoma leve de cortisol (anteriormente conocida como síndrome de Cushing subclínico)
Colaboradores
Autores
Maria Fleseriu, MD, FACE
Professor of Medicine (Endocrinology) and Neurological Surgery
Director
Pituitary Center
Oregon Health & Science University
Portland
OR
Declarações
MF is on the Endocrine Society's Board of Directors. She holds a research grant to the university for clinical studies as principal investigator for Crinetics and Sparrow Pharmaceuticals, and is an occasional scientific consultant for Crinetics, Recordati, Sparrow Pharmaceuticals, and Xeris Pharmaceuticals. MF is an author of several references cited in this topic.
Agradecimentos
Dr Maria Fleseriu would like to gratefully acknowledge Dr Ty Carroll and Dr James Findling, contributors to a previous version of this topic.
Declarações
TC is an author of a number of references cited in this topic. He is an investigator in clinical trials sponsored by Corcept. JF is an author of a number of references cited in this topic. He is a consultant for, and investigator in, clinical trials sponsored by Corcept and Novartis.
Revisores
Paul M. Stewart, FRCP FMedSci
Professor of Medicine
Director of Research
College of Medical and Dental Sciences
University of Birmingham
Honorary Consultant Physician
Queen Elizabeth Hospital
Birmingham
UK
Declarações
PMS declares that he has no competing interests.
Antoine Tabarin, MD
Head
Department of Endocrinology
University Hospital of Bordeaux
Pessac
France
Declarações
AT declares that he has no competing interests.
Liliana Contrersas, MD
Chief
Endocrine Research Department
Instituto de Investigaciones Médicas A. Lanari
University of Buenos Aires and IDIM-CONICET
Buenos Aires
Argentina
Declarações
LC declares that she has no competing interests.
Philip R. Orlander, MD
Professor of Medicine
Director
Division of Endocrinology, Diabetes & Metabolism
University of Texas Medical School
Houston
TX
Declarações
PRO declares that he has no competing interests.
Mouhammed Amir Habra, MD, FACP, FACE
Assistant Professor
Department of Endocrine Neoplasia and Hormonal Disorders
Division of Internal Medicine
University of Texas MD Anderson Cancer Center
Houston
TX
Disclosures
MAH declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Fleseriu M, Auchus R, Bancos I, et al. Consensus on diagnosis and management of Cushing's disease: a guideline update. Lancet Diabetes Endocrinol. 2021 Dec;9(12):847-75.Full text Abstract
Nieman LK, Biller BM, Findling JW, et al. Treatment of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015 Aug;100(8):2807-31.Full text Abstract
Feelders RA, Newell-Price J, Pivonello R, et al. Advances in the medical treatment of Cushing's syndrome. Lancet Diabetes Endocrinol. 2019 Apr;7(4):300-12. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Obesidad
- Síndrome metabólico
- Aldosteronismo primario
More DifferentialsGuidelines
- NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors
- Clinical practice guideline on the management of adrenal incidentalomas
More GuidelinesPatient information
Presión arterial alta: ¿qué tratamientos funcionan?
Síndrome de Cushing causado por un problema interno
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer