Summary
Definition
History and exam
Key diagnostic factors
- presencia de factores de riesgo
- mujeres en edad reproductiva
- menstruación irregular
- infertilidad
- hirsutismo
Other diagnostic factors
- acné
- sobrepeso u obesidad
- hipertensión
- caída del pelo del cuero cabelludo
- piel grasosa o sudoración excesiva
- acantosis pigmentaria
Risk factors
- antecedentes familiares del síndrome del ovario poliquístico (SOPQ)
- adrenarquía prematura
- obesidad
- bajo peso al nacer
- exposición del feto a los andrógenos
- disruptores endocrinos ambientales
Diagnostic tests
1st tests to order
- 17-hidroxiprogesterona sérica
- prolactina sérica
- hormona estimulante de la tiroides en suero
- prueba de tolerancia a la glucosa oral
- perfil lipídico en ayunas
Tests to consider
- niveles séricos de testosterona libre y total
- sulfato de deshidroepiandrosterona (DHEAS) en sangre
- androstenediona sérica
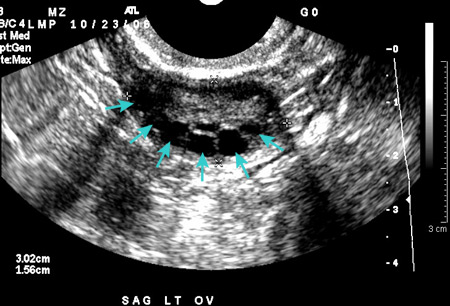
- ultrasonido pélvico
- hormona antimulleriana en suero
- monitorización de la temperatura corporal basal
- medición de progesterona en la fase lútea
- hormona luteinizante (LH) y hormona foliculoestimulante (FSH) séricas
- hemoglobina A1c o glucosa plasmática en ayunas
Treatment algorithm
con infertilidad cuando se desea fertilidad
sin deseo actual de fertilidad
Contributors
Authors
Mark O. Goodarzi, MD, PhD
Division of Endocrinology, Diabetes & Metabolism
Eris M. Field Chair in Diabetes Research
Professor of Medicine
Cedars-Sinai Medical Center
Los Angeles
CA
Disclosures
MOG has been reimbursed for one-time participation in an advisory board for Nestle Health Science on the topic of exocrine pancreatic dysfunction. MOG is an author of a number of references cited in this topic.
Peer reviewers
Antoni Duleba, MD
Professor
Department of Obstetrics and Gynecology
University of California Davis
Sacramento
CA
Disclosures
AD declares that he has no competing interests.
Richard S. Legro, MD
Professor
Department of Obstetrics and Gynecology
Penn State Hershey College of Medicine
Hershey
PA
Disclosures
RSL has been reimbursed by Serono for attending a medical conference and received a lecture fee, and has consulted for Ferring. He has received research funding from the NIH, the Commonwealth of Pennsylvania, and Parke Davis. He is an author of a number of references cited in this topic.
Cornelis B. (Nils) Lambalk, MD, PhD
Gynaecologist/Fertility Specialist
Division of Reproductive Medicine
Department of Obstetrics and Gynaecology
VU University Medical Centre
Amsterdam
The Netherlands
Divulgaciones
CBL declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Azziz R, Carmina E, Chen Z, et al. Polycystic ovary syndrome. Nat Rev Dis Primers. 2016 Aug 11;2:16057. Resumen
Teede HJ, Tay CT, Laven JJE, et al. Recommendations from the 2023 international evidence-based guideline for the assessment and management of polycystic ovary syndrome. J Clin Endocrinol Metab. 2023 Sep 18;108(10):2447-69.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Deficiencia de 21-hidroxilasa
- Disfunción tiroidea
- Hiperprolactinemia
Más DiferencialesGuías de práctica clínica
- International evidence-based guideline for the assessment and management of polycystic ovary syndrome
- ACOG practice bulletin: polycystic ovary syndrome
Más Guías de práctica clínicaFolletos para el paciente
Síndrome del ovario poliquístico: ¿cuáles son las opciones de tratamiento?
Síndrome del ovario poliquístico: ¿qué es?
Más Folletos para el pacienteInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad