Summary
Definition
History and exam
Key diagnostic factors
- presencia de factores de riesgo
- dolor torácico
- disnea
- taquipnea
- presíncope o síncope
- hipotensión (presión arterial sistólica <90 mmHg)
Other diagnostic factors
- sensación de ansiedad
- tos
- taquicardia
- fiebre
- hinchazón/sensibilidad unilateral de la pantorrilla
- hemoptisis
- aumento de la presión venosa yugular
- desplazamiento esternal
- componente pulmonar acentuado de S2
Risk factors
- diagnóstico de trombosis venosa profunda (TVP)
- cirugía mayor en los 3 meses anteriores
- hospitalización médica en los últimos 2 meses
- cáncer activo
- evento tromboembólico venoso previo
- traumatismo o fractura recientes
- mayor edad
- embarazo y posparto
- venas varicosas
- parálisis de las extremidades inferiores
- trombofilias hereditarias
- mutación del factor V de Leiden
- mutación del gen G20210A de la protrombina
- deficiencia de proteína C y proteína S
- deficiencia de antitrombina
- síndrome de anticuerpos antifosfolípidos
- comorbilidades médicas
- el uso de fármacos específicos
- obesidad (índice de masa corporal [IMC] ≥29 kg/kg/m²)
- tabaquismo
- viaje reciente de larga duración
- antecedentes familiares de tromboembolia venosa (TEV)
- cateterismo venoso central
Diagnostic investigations
1st investigations to order
- Criterios para descartar embolismo pulmonar (PERC)
- Criterios de Wells/puntuación de Ginebra/criterios YEARS
- Prueba del dímero D
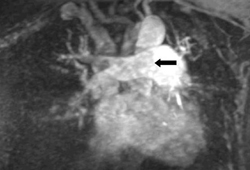
- angiografía pulmonar por tomografía computarizada (APTC) con detector múltiple
- gammagrafía de ventilación-perfusión (V/P)
- estudios de coagulación
- urea y creatinina, pruebas de función hepática
- hemograma completo (HC)
Investigations to consider
- Ecografía en el punto de atención (POCUS)
- radiografía de tórax
- angiografía por resonancia magnética (ARM)
- angiografía pulmonar
- ecocardiografía transtorácica (ETT)
- electrocardiograma (ECG)
- gasometría arterial (GSA)
- cribado de trombofilia
- ecografía
- troponina
Treatment algorithm
EP de alto riesgo (masiva) o alta probabilidad clínica de EP con shock o hipotensión (es decir, presión arterial sistólica < 90 mmHg), sin contraindicación para la anticoagulación o la trombólisis
riesgo alto o riesgo intermedio-alto, contraindicación para la anticoagulación o la trombólisis
riesgo intermedio-alto escala PESI/sPESI, sin contraindicación para la anticoagulación o la trombólisis
riesgo intermedio-bajo o riesgo bajo en la escala PESI/sPESI, sin contraindicación para la anticoagulación
riesgo intermedio-bajo o riesgo bajo en la escala PESI/sPESI, con contraindicación para la anticoagulación
EP confirmada: provocada
EP confirmada: no provocada
EP confirmada: embarazada
EP confirmada: asociada al cáncer
EP confirmada: EP recurrente durante el tratamiento con anticoagulación
Contributors
Authors
Scott Stevens, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor of Medicine
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Disclosures
SS declares that he has no competing interests.
Scott C. Woller, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor of Medicine
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Disclosures
SCW declares that he is expecting to receive funding of an investigator initiated grant from Janssen Pharmaceuticals to Intermountain Health with no direct compensation to himself for research in the sum of $500,000 in 2024.
Gabriel V. Fontaine, PharmD, MBA, BCPS
Clinical Pharmacy Manager
Critical Care and Emergency Medicine
Advanced Clinical Pharmacist
Neuroscience Critical Care
Intermountain Medical Center
Murray
UT
Disclosures
GVF has received consulting fees and honoraria from AstraZeneca, Chiesi, and Anticoagulation Forum.
Acknowledgements
Dr Scott M. Stevens, Dr Scott C. Woller, and Dr Gabriel V. Fontaine would like to gratefully acknowledge Drs Geno Merli, Luis H. Eraso, Taki Galanis, Geoffrey Ouma, Miguel Angel de Gregorio, Alicia Laborda, and Seth W. Clemens, previous contributors to this topic.
Disclosures
GM has received grants or research support from BMS, J&J, Sanofi-Aventis, Portola, and Janssen; he has served as a Scientific Consultant for BMS, J&J, and Sanofi-Aventis. LHE, TG, GO, MAG, AL, and SWC declare that they have no competing interests.
Peer reviewers
Keith Wille, MD, MSPH
Associate Professor of Medicine
University of Alabama at Birmingham
Birmingham
AL
Disclosures
KW declares that he has no competing interests.
John R. Charpie, MD, PhD
Associate Professor of Pediatrics
Medical Director
Pediatric Cardiothoracic Intensive Care Unit
University of Michigan Congenital Heart Center
C.S. Mott Children's Hospital
Ann Arbor
MI
Disclosures
JRC declares that he has no competing interests.
Sanjeev Wasson, MD
Advanced Clinical Fellow
Cleveland Clinic Foundation
Cleveland
OH
Disclosures
SW declares that he has no competing interests.
David Jimenez, MD, PhD
Respiratory Physician and Associate Professor
Ramón y Cajal Hospital and Alcalá de Henares University
Respiratory Department and Medicine Department
Madrid
Spain
Disclosures
DJ has received consulting fees from Boehringer Ingelheim, Bayer, Leo-Pharm, and Rovi, and lecture fees from Sanofi Aventis.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020 Jan 21;41(4):543-603.Full text
Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. 2021 Dec;160(6):e545-608.Full text Abstract
American College of Radiology. ACR Appropriateness Criteria®: suspected pulmonary embolism. 2022 [internet publication].Full text
Bates SM, Rajasekhar A, Middeldorp S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018 Nov 27;2(22):3317-59.Full text Abstract
Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: compendium and review of CHEST guidelines 2012-2021. Chest. 2024 Aug;166(2):388-404.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Angina, inestable
- infarto de miocardio, sin elevación del segmento ST (IMSEST)
- Infarto de miocardio, elevación del segmento ST (IMCEST)
More DifferentialsGuidelines
- NCCN clinical practice guidelines in oncology: cancer-associated venous thromboembolic disease
- ACR appropriateness criteria: imaging for pulmonary embolism, known clot
More GuidelinesPatient information
Embolia pulmonar: ¿qué es?
Embolia pulmonar: ¿qué tratamiento funciona?
More Patient informationCalculators
Puntuación Pulmonary Embolism Wells Score
Escala de Ginebra revisada para la estimación de la probabilidad clínica de embolia pulmonar en adultos
More CalculatorsVideos
Demostración animada de la intubación traqueal
Demostración animada de la ventilación bolsa-válvula-máscara
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer
