Summary
Definition
History and exam
Principais fatores diagnósticos
- pallor
- jaundice
Outros fatores diagnósticos
- fatigue
- shortness of breath
- dizziness
- splenomegaly
- active infections
- episodic dark urine (hemoglobinuria)
- triggered by exposure to cold
Fatores de risco
- autoimmune disorders
- lymphoproliferative disorders
- prosthetic heart valve
- family origin in Mediterranean, Middle East, Africa, or Southeast Asia
- family history of hemoglobinopathy or red blood cell membrane defects
- paroxysmal nocturnal hemoglobinuria
- recent exposure to cephalosporins, penicillins, quinine derivatives, or nonsteroidal anti-inflammatory drugs
- recent exposure to naphthalene or fava beans
- thermal injury
- exceptional exertion
- recent exposure to nitrites, dapsone, ribavirin, or phenazopyridine
- recent paraquat ingestion
- malaria
- babesiosis
- bartonellosis
- leishmaniasis
- Clostridium perfringens infection
- Haemophilus influenzae type B infection
- liver disease
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- CBC
- MCHC
- reticulocyte count
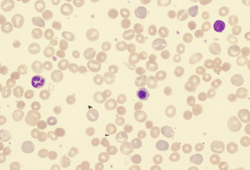
- peripheral smear
- unconjugated (indirect) bilirubin
- LDH
- haptoglobin
- urinalysis
Investigações a serem consideradas
- direct antiglobulin test (Coombs)
- creatinine, BUN
- LFTs
- Donath-Landsteiner antibody
- Hb electrophoresis
- flow cytometry for CD55/CD59
- glucose-6-phosphate dehydrogenase (G6PD) fluorescent spot test and spectrophotometry
- antinuclear antibody
Algoritmo de tratamento
acquired: direct antiglobulin test (Coombs) positive
acquired: direct antiglobulin test (Coombs) negative
inherited disorders
Colaboradores
Autores
John Densmore, MD, PhD
Associate Professor of Clinical Medicine
Department of Medicine
University of Virginia
Charlottesville
VA
Declarações
JD declares that he has no competing interests.
Agradecimentos
Dr John Densmore would like to gratefully acknowledge Dr Michelle Loch, a previous contributor to this monograph. ML declares that she has no competing interests.
Revisores
Pasquale Niscola, MD
Hematology Unit
Sant'Eugenio Hospital
Rome
Italy
Declarações
PN declares that he has no competing interests.
Alan Lichtin, MD
Staff Hematologist-Oncologist
Hematologic Oncology and Blood Disorders
Cleveland Clinic
Associate Professor
Internal Medicine
Cleveland Clinic Lerner College of Medicine
Cleveland
OH
Declarações
AL declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Go RS, Winters JL, Kay NE. How I treat autoimmune hemolytic anemia. Blood. 2017 Jun 1;129(22):2971-9 Resumo
Hill QA, Stamps R, Massey E, et al. The diagnosis and management of primary autoimmune haemolytic anaemia. Br J Haematol. 2017 Feb;176(3):395-411.Texto completo Resumo
Hill QA, Stamps R, Massey E, et al. Guidelines on the management of drug-induced immune and secondary autoimmune, haemolytic anaemia. Br J Haematol. 2017 Apr;177(2):208-20.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Anemia due to blood loss
- Underproduction anemia
- Transfusion reaction
Mais Diagnósticos diferenciaisDiretrizes
- Diagnosis and treatment of autoimmune hemolytic anemia in adults
- Recommendations regarding splenectomy in hereditary hemolytic anemias
Mais DiretrizesVideos
Venepuncture and phlebotomy: animated demonstration
Peripheral intravascular catheter: animated demonstration
Mais vídeosConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal