Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- abdominal fullness or discomfort
- splenomegaly
Outros fatores diagnósticos
- weakness and fatigue
- unexplained weight loss
- bruising and bleeding
- pallor
- recurrent infections
- hepatomegaly
- lymphadenopathy
- neurologic findings
- associated systemic immunologic disorders
Fatores de risco
- middle age
- male sex
- white ancestry
- western hemisphere location
- environmental exposures
- genetic predisposition
- Epstein-Barr virus
- infectious mononucleosis
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- CBC with differential
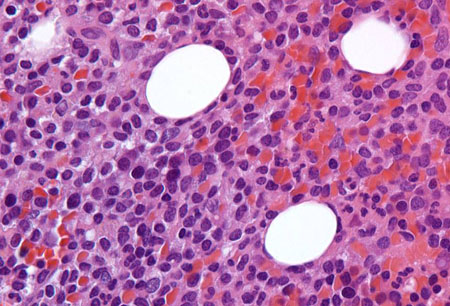
- peripheral blood smear
- bone marrow trephine biopsy and aspiration (morphology assessment)
- immunophenotyping (immunohistochemistry or flow cytometry)
- comprehensive metabolic panel
- serum lactate dehydrogenase (LDH)
- viral serology for hepatitis B and C
Investigações a serem consideradas
- molecular analysis (for BRAF V600E mutation or IGHV4-34 rearrangement)
- CT chest, abdomen, and pelvis
Algoritmo de tratamento
no indication(s) for treatment
indication(s) for treatment present: without splenic rupture or massive splenomegaly or marked thrombocytopenia precluding chemotherapy
indication(s) for treatment present: with massive symptomatic splenomegaly or splenic rupture or marked thrombocytopenia precluding chemotherapy
early relapse (<2 years) or refractory disease
late relapse (≥2 years)
Colaboradores
Autores
Ambuj Kumar, MD, MPH
Professor
USF Health Office of Research
Department of Internal Medicine, College of Medicine
Moffitt Cancer Center & Research Institute, Department of Health Outcomes & Behavior
University of South Florida
Tampa
FL
Declarações
AK declares that he has no competing interests.
Mohamed A. Kharfan-Dabaja, MD, MBA, FACP
Professor
Division of Hematology-Oncology
Blood and Marrow Transplantation Program
Mayo Clinic
Jacksonville
FL
Declarações
MKD declares that he has no competing interests.
Agradecimentos
Dr Ambuj Kumar and Dr Mohamed Kharfan-Dabaja would like to gratefully acknowledge Dr Benjamin Djulbegovic, a previous contributor to this topic.
Declarações
BD declares that he has no competing interests.
Revisores
Daniel Catovsky, MD, FRCP, FRCPath, DSc, FMedSc
Consultant Haemato-Oncologist
Section of Haemato-Oncology
Brookes Lawley Institute of Cancer
Sutton
UK
Declarações
DC declares that he has no competing interests.
Roger Lyons, MD
Clinical Professor of Medicine
University of Texas Health Science Center San Antonio
San Antonio
TX
Declarações
RL declares that he has no competing interests.
Rebecca Connor, MD
Chief Fellow
Section of Hematology and Oncology
Department of Internal Medicine
Wake Forest University Baptist Medical Center
Winston-Salem
NC
Declarações
RC declares that she has no competing interests.
Claire Dearden, BSc, MD, FRCP, FRCPath
Consultant Haematologist
The Royal Marsden Hospital
Sutton
Surrey
UK
Declarações
CD declares that she has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Parry-Jones N, Joshi A, Forconi F, et al. Guideline for diagnosis and management of hairy cell leukaemia (HCL) and hairy cell variant (HCL-V). Br J Haematol. 2020 Dec;191(5):730-7.Texto completo Resumo
Troussard X, Maître E, Paillassa J. Hairy cell leukemia 2024: update on diagnosis, risk-stratification, and treatment - annual updates in hematological malignancies. Am J Hematol. 2024 Apr;99(4):679-96.Texto completo Resumo
Grever MR, Abdel-Wahab O, Andritsos LA, et al. Consensus guidelines for the diagnosis and management of patients with classic hairy cell leukemia. Blood. 2017 Feb 2;129(5):553-60.Texto completo Resumo
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: hairy cell leukemia [internet publication].Texto completo
Robak T, Matutes E, Catovsky D, et al. Hairy cell leukaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015 Sep;26(suppl 5):v100-7.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Chronic lymphocytic leukemia (CLL)
- Mantle cell lymphoma
- Prolymphocytic leukemia
Mais Diagnósticos diferenciaisDiretrizes
- NCCN clinical practice guidelines in oncology: hairy cell leukemia
- Guideline for diagnosis and management of hairy cell leukaemia (HCL) and hairy cell variant (HCL-V)
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal
