Summary
Definition
History and exam
Key diagnostic factors
- pulse rate <50 bpm
- age >70 years
- use of known causative medications
- presence of known underlying cause
- dizziness/lightheadedness
- syncope
- fatigue
- exercise intolerance
- shortness of breath
- cannon a-waves in jugular venous pulse
- jugular venous distension
Other diagnostic factors
- increased intracranial pressure
- abnormal heart sounds
- abdominal or lower extremity edema
- hypotension
- mental status changes
- pallor
- extremities cool to touch
- hypothermia
- chest pain
- rashes
- thyroid goiter
Risk factors
- use of known causative medications
- age >70 years
- recent myocardial infarction
- surgery
- percutaneous valve replacement procedures
- hypothyroidism
- electrolyte disorders
- acidosis
- infections
- exposure to toxins
- hypothermia
- infiltrative diseases
- sleep-disordered breathing
- epilepsy
Diagnostic tests
1st tests to order
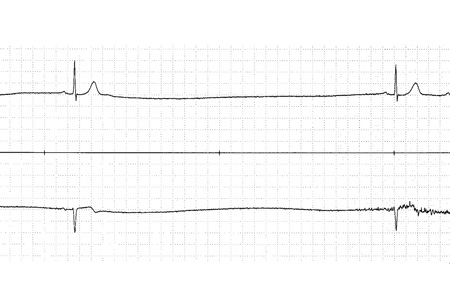
- 12-lead ECG
- Holter monitoring
- event monitor/mobile cardiac telemetry
- exercise testing
- carotid sinus massage
- echocardiogram
- thyroid function tests
- basic metabolic panel
- arterial blood gas
- cardiac biomarkers
- serum digoxin level
- serum creatinine
Tests to consider
- implantable-loop recorder
- tilt-table testing
- Lyme titers
- electrophysiology testing
- nocturnal pulse oximetry or overnight polysomnography
Treatment algorithm
hemodynamically unstable
hemodynamically stable: sinus node dysfunction
hemodynamically stable: acquired atrioventricular block
hemodynamically stable: congenital atrioventricular block
hemodynamically stable: vagally mediated bradycardia
hemodynamically stable: bradycardia associated with neurologic disorders
Contributors
Authors
Brian Olshansky, MD, FAHA, FACC, FHRS, FESC

Professor Emeritus
University of Iowa
Iowa City
Adjunct Professor
Des Moines University
Electrophysiologist
Covenant Hospital
Waterloo
IA
VA Hospital
Iowa City
IA
CGH Medical Center
Sterling
IL
Disclosures
BO declares that he has no competing interests.
Sandeep Saha, MD, MS, FACC, FHRS
Consultant, Cardiology and Cardiac Electrophysiology
Oregon Heart Center
Salem
OR
Disclosures
SS is a consultant for Medtronic and St Jude Medical. He is on the speakers' bureau and serves as an advisory board member for Medtronic. None of these activities are relevant to the content of this topic.
Rakesh Gopinathannair, MD, MA, FAHA, FACC, FHRS

Director, Cardiac Electrophysiology Laboratories
Kansas City Heart Rhythm Institute and Research Foundation
EP Medical Director
Research Medical Center, HCA Midwest Health
Overland Park
KS
Clinical Professor of Medicine
University of Missouri-Columbia
Columbia
MO
Disclosures
RG is a consultant for St. Jude Medical, Biotrionik, and Boston Scientific. He is on the speakers' bureau for Pfizer Inc. and Zoll Medical. He serves as a physician advisor for HealthTrust PG and AltaThera Pharma, and PaceMate. None of these activities are relevant to the content of this topic.
Acknowledgements
Professor Brian Olshansky, Dr. Sandeep Saha, and Professor Rakesh Gopinathannair would also like to acknowledge Dr Giselle Statz, Dr Renee M. Sullivan, Dr Weiwei Li, Dr Alexander Mazur, and Dr Chirag M. Sandesara, previous contributors to this topic.
Disclosures
GS, RMS, WL, AM, and CMS declare that they have no competing interests.
Peer reviewers
Nora Goldschlager, MD
Professor of Clinical Medicine
University of California
Chief
Clinical Cardiology
San Francisco General Hospital
Director
Coronary Care Unit
ECG Laboratory and Pacemaker Clinic
San Francisco
CA
Disclosures
NG declares that she has no competing interests.
Paul Heidenreich, MD
Associate Professor of Medicine
Stanford University
Stanford
CA
Disclosures
PH declares that he has no competing interests.
Juan M. Sztajzel, MD
Cardiology Center and Medical Polyclinics
University Hospital Geneva
Geneva
Switzerland
Disclosures
JMS declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Mangrum JM, DiMarco JP. The evaluation and management of bradycardia. N Engl J Med. 2000 Mar 9;342(10):703-9. Abstract
Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Aug 20;74(7):e51-156.Full text Abstract
Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020 Oct 20;142(16_suppl_2):S366-S468.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Ventricular bigeminy
- Frequent premature ventricular contractions (PVCs)
- Atrial fibrillation
More DifferentialsGuidelines
- 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy
- 2020 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care
More GuidelinesPatient information
Bradycardia
More Patient informationVideos
How to perform an ECG: animated demonstration
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer