Tachycardia, generally defined as a heart rate ≥100 bpm, can be a normal physiologic response to a systemic process or a manifestation of underlying pathology.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-115.
https://www.sciencedirect.com/science/article/pii/S0735109715058404?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
[2]Katritsis DG, Boriani G, Cosio FG, et al. European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardiaca y Electrofisiologia (SOLAECE). Europace. 2017 Mar 1;19(3):465-511.
https://academic.oup.com/europace/article/19/3/465/2631183
http://www.ncbi.nlm.nih.gov/pubmed/27856540?tool=bestpractice.com
The normal heart rate varies with age. The normal sinus rate in infants is 110 to 150 bpm, which gradually slows with age.[3]Bjerregaard P. Mean 24 hour heart rate, minimal heart rate and pauses in healthy subjects 40-79 years of age. Eur Heart J. 1983 Jan;4(1):44-51.
http://www.ncbi.nlm.nih.gov/pubmed/6339245?tool=bestpractice.com
Classification of tachyarrhythmia
Several methods of classification of tachyarrhythmia are helpful in organizing and evaluating tachycardias. These include: sinus versus non-sinus causes; atrial versus ventricular arrhythmias; narrow- versus wide-complex tachycardias; regular versus irregular arrhythmias; and classification based on the site of origin of the arrhythmia.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-115.
https://www.sciencedirect.com/science/article/pii/S0735109715058404?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
Sinus versus non-sinus causes
Sinus tachycardia is a common cause of tachycardia that can often be mistaken for an arrhythmia. Diagnosis depends on the P-wave morphology and the setting in which it occurs. Because each impulse originates in the sinoatrial node, the ECG shows a P wave preceding each QRS interval with a normal P-wave axis. In most cases, a secondary cause of sinus tachycardia can be identified. A careful assessment is important, to evaluate whether the sinus rate is appropriate for the clinical situation. Sinus tachycardia can be mistaken for other supraventricular arrhythmias, including atrial flutter, particularly with rapid tachyarrhythmias (when P waves are difficult to distinguish or when ectopic atrial foci originate near the sinoatrial node, such as near the superior vena cava or upper crista terminalis).
Atrial versus ventricular arrhythmia
Whether the arrhythmia originates from the atrium or the ventricle is usually dependent on whether the QRS complex is wide or narrow, and on the atrial:ventricular relationship. Atrial arrhythmias usually conduct to the ventricle through the His-Purkinje system and result in a narrow QRS complex. Some overlap may occur when conduction occurs with aberrancy (left or right bundle branch block), if there is pre-excitation, and in the presence of antiarrhythmic agents that may slow conduction (sodium channel blockers). If P waves are discernible, an atrial:ventricular relationship of <1 is highly suggestive of a ventricular origin, whereas a relationship >1 is highly suggestive of an atrial origin. A 1:1 atrial:ventricular relationship can occur with both atrial and ventricular arrhythmias.
Narrow versus wide QRS complex
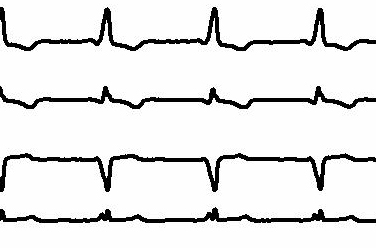
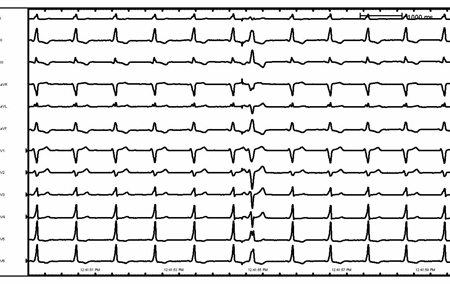
Classification can also be based on whether there is a narrow- (QRS interval <120 ms) or wide- (QRS interval >120 ms) complex tachycardia. Narrow-QRS-complex tachycardia suggests that anterograde conduction and thus depolarization of the ventricle occurs through the atrioventricular (AV) node and His-Purkinje system. A wide-complex tachycardia suggests that conduction through the ventricle occurs through the slower myocyte-to-myocyte connections (because of either AV conduction via an accessory pathway or a ventricular origin) and can be seen even with sinus rhythm. However, atrial tachyarrhythmias that conduct aberrantly may present as a wide-complex tachycardia.[Figure caption and citation for the preceding image starts]: Sinus rhythm with preexcitationFrom the collection of Robert W. Rho, MD; used with permission [Citation ends].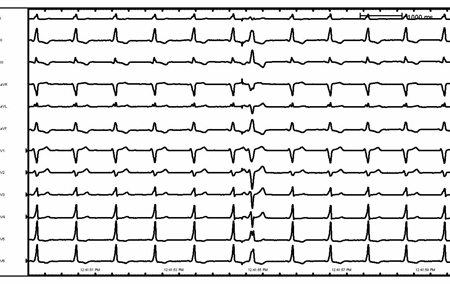 [Figure caption and citation for the preceding image starts]: Sinus rhythm with preexcitation (detail)From the collection of Robert W. Rho, MD; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sinus rhythm with preexcitation (detail)From the collection of Robert W. Rho, MD; used with permission [Citation ends].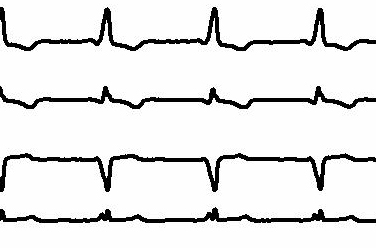
Regular versus irregular rhythm
Whether a rhythm is regular or irregular is easy to determine clinically and can help guide diagnosis of the tachyarrhythmia. An irregular rhythm is defined as a beat-to-beat R-R variability of more than 30 ms. In general, irregular narrow-complex arrhythmias include: atrial fibrillation, atrial flutter with variable conduction, and multifocal atrial tachycardia. An irregular wide-complex tachycardia may be due to pre-excited atrial fibrillation (due to a rapidly anterograde-conducting bypass tract), polymorphic ventricular tachycardia and atrial fibrillation, or multifocal atrial tachycardia conducting with aberrancy.
Site of origin
Tachyarrhythmias can be classified according to the site of origin: atrial, junctional, or ventricular:
Atrial impulses are characterized by initial depolarization of the atrium, from a single focus, such as sinus tachycardia or atrial tachycardia; macro reentry around an anatomic obstacle, such as in typical atrial flutter; or from multiple wavelets of reentry, such as atrial fibrillation.
Arrhythmias that originate at the level of the junction of the atrium and ventricle (AV node and/or proximal His bundle), such as AV nodal reentrant tachycardia or junctional ectopic tachycardia, are characterized by depolarization of the ventricle and retrograde atrial activation (if present), manifested by a retrograde P wave.
Arrhythmias that originate from the ventricle may originate from the distal His-Purkinje system or ventricular myocardium. The site of origin within the ventricle further defines some arrhythmias within the ventricle. Examples include right ventricular outflow tract ventricular tachycardia and bundle branch reentry ventricular tachycardia. Hemodynamic stability is not a helpful factor in differentiating atrial and ventricular arrhythmias. Some cases of ventricular tachycardia may be initially well tolerated hemodynamically. Misdiagnosis and inappropriate treatment (i.e., calcium channel blockers) may have catastrophic consequences.
When a patient with a wide-complex tachycardia is being evaluated and the diagnosis is not certain, the arrhythmia must be initially regarded as ventricular tachycardia until it is proved to be otherwise.
Epidemiology
Sinus tachycardia is the most common cause of sustained tachycardia, as it is usually a normal physiologic response to emotional or physical stimulation.[4]Mayuga KA, Fedorowski A, Ricci F, et al. Sinus tachycardia: a multidisciplinary expert focused review. Circ Arrhythm Electrophysiol. 2022 Sep;15(9):e007960.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9523592
http://www.ncbi.nlm.nih.gov/pubmed/36074973?tool=bestpractice.com
Atrial fibrillation is the most common arrhythmia in clinical practice, with an estimated global prevalence of 52.55 million in 2021.[5]Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024 Jan 2;149(1):e1-156.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11095842
http://www.ncbi.nlm.nih.gov/pubmed/38033089?tool=bestpractice.com
[6]Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001303
http://www.ncbi.nlm.nih.gov/pubmed/39866113?tool=bestpractice.com
Up to 9% of patients aged 80 years or older have atrial fibrillation.[7]Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 9;285(18):2370-5.
http://jama.ama-assn.org/cgi/reprint/285/18/2370
http://www.ncbi.nlm.nih.gov/pubmed/11343485?tool=bestpractice.com
[8]Murphy NF, Simpson CR, Jhund PS, et al. A national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in Scotland. Heart. 2007 May;93(5):606-12.
https://www.doi.org/10.1136/hrt.2006.107573
http://www.ncbi.nlm.nih.gov/pubmed/17277353?tool=bestpractice.com
As the proportion of older people in the population increases, the number with atrial fibrillation is likely to increase significantly.
In the US, the prevalence of atrial fibrillation is estimated to increase from approximately 5.2 million in 2010 to 12.1 million in 2030.[6]Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001303
http://www.ncbi.nlm.nih.gov/pubmed/39866113?tool=bestpractice.com
[9]Colilla S, Crow A, Petkun W, et al. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013 Oct 15;112(8):1142-7.
https://www.ajconline.org/article/S0002-9149(13)01288-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23831166?tool=bestpractice.com
In the European Union, prevalence of atrial fibrillation (in adults ages >55 years) is projected to increase from 8.8 million in 2010 to 17.9 million by 2060.[10]Krijthe BP, Kunst A, Benjamin EJ, et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J. 2013 Sep;34(35):2746-51.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858024
http://www.ncbi.nlm.nih.gov/pubmed/23900699?tool=bestpractice.com
The incidence of atrial flutter has been reported as 88 cases per 100,000 person-years; it is more common in men, with increasing age, and in those with heart failure or COPD.[11]Granada J, Uribe W, Chyou P, et al. Incidence and predictors of atrial flutter in the general population. J Am Coll Cardiol. 2000 Dec;36(7):2242-6.
http://www.ncbi.nlm.nih.gov/pubmed/11127467?tool=bestpractice.com
[12]Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. Eur Heart J. 2020 Feb 1;41(5):655-720.
https://academic.oup.com/eurheartj/article/41/5/655/5556821
PSVT, defined as intermittent supraventricular tachycardia (AV node reentry tachycardia, AV reciprocating tachycardia, or atrial tachycardia) has an incidence of 57.8 cases per 100,000 person-years and a prevalence of 1.26 million people in the US.[13]Rehorn M, Sacks NC, Emden MR, et al. Prevalence and incidence of patients with paroxysmal supraventricular tachycardia in the United States. J Cardiovasc Electrophysiol. 2021 Aug;32(8):2199-206.
http://www.ncbi.nlm.nih.gov/pubmed/34028109?tool=bestpractice.com
Females are twice as likely to develop PSVT, and the incidence is five times greater in people older than 65 years compared with younger people.[14]Orejarena L, Vidaillet HJ, DeStefano F, et al. Paroxysmal supraventricular tachycardia in the general population. J Am Coll Cardiol. 1998 Jan;31(1):150-7.
https://www.sciencedirect.com/science/article/pii/S0735109797004221
http://www.ncbi.nlm.nih.gov/pubmed/9426034?tool=bestpractice.com
Most cases of supraventricular tachycardia are due to AV nodal reentrant tachycardia (60% of cases); the remainder are due to AV reciprocating tachycardia (30%) and atrial tachycardia (10%).[15]Trohman RG. Supraventricular tachycardia: implications for the intensivist. Crit Care Med. 2000 Oct;28(10 Suppl):N129-35.
http://www.ncbi.nlm.nih.gov/pubmed/11055681?tool=bestpractice.com
The prevalence of inappropriate sinus tachycardia is not well known and the underlying mechanisms are likely to be multifactorial, but patients are often young (age 15 to 50 years) and female.[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-115.
https://www.sciencedirect.com/science/article/pii/S0735109715058404?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/26409259?tool=bestpractice.com
[2]Katritsis DG, Boriani G, Cosio FG, et al. European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardiaca y Electrofisiologia (SOLAECE). Europace. 2017 Mar 1;19(3):465-511.
https://academic.oup.com/europace/article/19/3/465/2631183
http://www.ncbi.nlm.nih.gov/pubmed/27856540?tool=bestpractice.com
[16]Brady PA, Low PA, Shen WK. Inappropriate sinus tachycardia, postural orthostatic tachycardia syndrome, and overlapping syndromes. Pacing Clin Electrophysiol. 2005 Oct;28(10):1112-21.
http://www.ncbi.nlm.nih.gov/pubmed/16221272?tool=bestpractice.com
The prevalence of ventricular tachyarrhythmia is highly dependent on its type and duration. In patients with a history of previous MI, the incidence of sustained monomorphic ventricular tachyarrhythmia depends on the size of the infarction and the overall left ventricular function.


შედით სისტემაში ან გამოიწერეთ BMJ Best Practice