Summary
Definition
History and exam
Key diagnostic factors
- advanced age
- ethnicity
- previous osteoporotic vertebral compression fracture
- acute back pain
- asymptomatic
Other diagnostic factors
- history of long-term corticosteroid use
- bone-losing medications
- kyphotic deformity
- loss of lumbar lordosis
- localized tenderness
- loss of standing height
- loss of sagittal balance
Risk factors
- older age
- previous osteoporotic vertebral compression fracture
- low body weight
- recent weight loss
- family history of low bone mass/osteoporotic fractures
- smoking
- white or Asian race
- postmenopausal status
- secondary amenorrhea
- alcohol (>2 units/day)
- corticosteroid use
- glucocorticoid excess
- hyperthyroidism
- vitamin D deficiency
- low calcium intake
- rheumatoid arthritis and other autoimmune connective tissue diseases
- endocrine disorders (e.g., hypogonadism, hyperparathyroidism, hyperprolactinemia, acromegaly, hypercortisolism, hyperthyroidism)
- gastrointestinal diseases (e.g., inflammatory bowel disease, celiac disease, malabsorption syndromes, post-bariatric surgery)
- liver diseases (e.g., biliary sclerosis, sclerosing cholangitis, alcoholic cirrhosis, autoimmune hepatitis)
- dietary disorders (e.g., anorexia nervosa/bulimia, inadequate diet, total parenteral nutrition)
- neurologic disorders (e.g., stroke, multiple sclerosis, Parkinson disease, spinal cord injury, long-term immobilization)
- renal disease
- type 1 diabetes mellitus
- organ transplantation
- bone-losing medications
Diagnostic tests
1st tests to order
- plain x-rays
Tests to consider
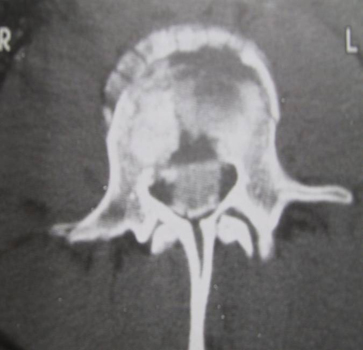
- CT spine
- MRI spine
- technetium-99m (Tc-99m) whole-body bone scan (bone scintigraphy)
- single-photon emission computed tomography (SPECT)/CT
- bone densitometry scan
- CT myelogram
- CBC
- bone profile (including serum calcium and alkaline phosphatase)
- C-reactive protein
- blood cultures
Treatment algorithm
anterior column involvement only
multiple column involvement
Contributors
Authors
Nasir A. Quraishi, LLM, FRCS
Consultant Spine Surgeon & Honorary Clinical Associate Professor
Centre for Spinal Studies and Surgery
Queen’s Medical Centre
Nottingham
UK
Disclosures
NAQ declares that he has no competing interests.
Opinder Sahota, FRCP, DM, FHEA
Professor of Orthogeriatric Medicine & Consultant Physician
Queen's Medical Centre
Nottingham University Hospitals NHS Trust
Nottingham
UK
Disclosures
OS declares that he has no competing interests.
Acknowledgements
Dr Nasir A. Quraishi and Dr Opinder Sahota would like to gratefully acknowledge Dr Jeremy Fairbank, previous contributor to this topic.
Peer reviewers
Kee D. Kim, MD
Professor of Neurological Surgery
University of California
Davis
CA
Disclosures
KDK declares that he has no competing interests.
Micky Malhotra, MBBS, DTCD, MD, MRCP
Consultant Physician
Wrightington, Wigan & Leigh NHS Foundation Trust
Wigan
UK
Disclosures
MM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
American College of Radiology. ACR appropriateness criteria: management of vertebral compression fractures. 2022 [internet publication].Full text
LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-102.Full text Abstract
The North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022 Jul 1;29(7):767-94.Full text Abstract
North American Spine Society. Diagnosis and treatment of adults with osteoporotic vertebral compression fractures. Sep 2024 [internet publication].Full text
Royal Osteoporosis Society. Guidance for the management of symptomatic vertebral fragility fractures. May 2022 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.

Differentials
- Muscular pain
- Spinal stenosis
- Pathologic fracture
More DifferentialsGuidelines
- Appropriate use criteria: osteoporotic vertebral fracture
- Appropriate use criteria: neoplastic vertebral fracture
More GuidelinesPatient information
Osteoporosis: questions to ask your doctor
Osteoporosis: what is it?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer