Summary
Differentials
Common
- Familial short stature (genetic short stature)
- Constitutional delay of growth and development
- Idiopathic short stature
- Small for gestational age (SGA) without catch-up growth by 2 years of age
Uncommon
- Growth hormone (GH) deficiency
- Hypothyroidism
- Cushing syndrome
- GH insensitivity (Laron syndrome)
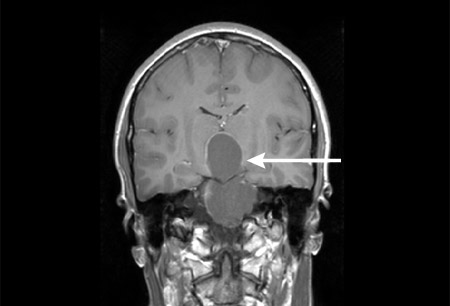
- Craniopharyngioma
- Turner syndrome
- Noonan syndrome
- Russell-Silver syndrome
- Trisomy 21
- Prader-Willi syndrome (PWS)
- DiGeorge syndrome (velocardiofacial syndrome)
- Celiac disease
- Cystic fibrosis (CF)
- Asthma (moderate or severe)
- Chronic heart disease (congenital or acquired)
- Diabetes mellitus
- Chronic kidney failure
- Juvenile idiopathic arthritis (JIA)
- Crohn disease
- Ulcerative colitis
- Malignancy
- Renal tubular acidosis
- Rickets
- Skeletal dysplasias (e.g., achondroplasia, hypochondroplasia, osteogenesis imperfecta)
- Spinal disorders (irradiation, surgery, congenital deformities)
- Psychosocial deprivation (abuse, neglect, starvation, institutionalization)
- Anorexia nervosa
- Bulimia nervosa
- Fetal alcohol syndrome
- Stimulant medications for ADHD
Contributors
Authors
Renee Bargman, MS, MD

Pediatric Endocrinology
NYC Health and Hospitals/SUNY Downstate Medical Center
Brooklyn
NY
Disclosures
RB declares that she has no competing interests.
Acknowledgements
Dr Renee Bargman would like to gratefully acknowledge Dr Maria Vogiatzi, a previous contributor to this topic.
Peer reviewers
Ian Marshall, MD
Chief of the Division of Pediatric Endocrinology
Assistant Professor
UMDNJ-Robert Wood Johnson Medical School
New Brunswick
NY
Disclosures
IM declares that he has no competing interests.
Raphael David, MD
Professor of Pediatrics
Director
Pediatric Endocrinology
New York University Medical Center
New York
NY
Disclosures
RD declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Wit JM, Kamp GA, Oostdijk W, et al. Towards a rational and efficient diagnostic approach in children referred for growth failure to the general paediatrician. Horm Res Paediatr. 2019;91(4):223-40.Full text Abstract
Cooke R, Goulet O, Huysentruyt K, et al. Catch-up growth in infants and young children with faltering growth: expert opinion to guide general clinicians. J Pediatr Gastroenterol Nutr. 2023 Jul 1;77(1):7-15.Full text Abstract
Cohen P, Rogol AD, Deal CL, et al. Consensus statement on the diagnosis and treatment of children with idiopathic short stature: a summary of the Growth Hormone Research Society, the Lawson Wilkins Pediatric Endocrine Society, and the European Society for Paediatric Endocrinology Workshop. J Clin Endocrinol Metab. 2008 Nov;93(11):4210-7.Full text Abstract
Bryant J, Baxter L, Cave CB, et al. Recombinant growth hormone for idiopathic short stature in children and adolescents. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD004440.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Use of this content is subject to our disclaimer