Summary
Definition
History and exam
Key diagnostic factors
- scarred uterus
- presence of other risk factors
- painless vaginal bleeding
- absence of cervical/vaginal causes of bleeding on speculum examination
Other diagnostic factors
- previous ultrasound anomaly in first trimester
- lack of uterine tenderness
- low blood pressure and tachycardia
Risk factors
- advanced maternal age
- multiple previous pregnancies
- smoking
- previous miscarriage
- previous induced abortion
- other placental abnormalities
- short interpregnancy intervals
- illicit drug use
- uterine scarring (most commonly due to prior cesarean section)
- infertility treatments
- prior placenta previa
Diagnostic tests
1st tests to order
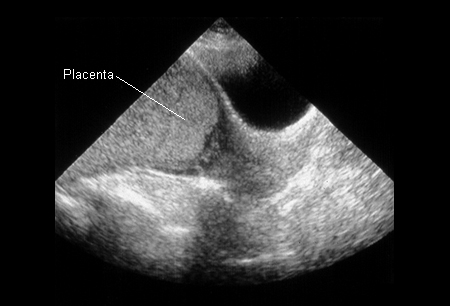
- uterine ultrasound with color flow Doppler analysis
- CBC
- type and crossmatch
Tests to consider
- MRI placenta
- INR/PTT, fibrinogen, and fibrinogen degradation products
- Kleihauer-Betke test
Treatment algorithm
bleeding with unknown placental position
bleeding with known placenta previa
placenta previa with no bleeding
with miscarriage or elective termination
Contributors
Authors
Janet R. Albers, MD

Professor
Department Chair
Family and Community Medicine
Southern Illinois University School of Medicine
Springfield
IL
Disclosures
JRA declares that she has no competing interests.
Thomas H. Miller, MD
Professor
Clinical Family and Community Medicine
Associate Chairman - Western Region
Southern Illinois University School of Medicine
Springfield
IL
Disclosures
THM declares that he has no competing interests.
Acknowledgements
Dr Janet R. Albers and Dr Thomas H. Miller would like to gratefully acknowledge Dr Robert Ewart and Dr Matthew Hagermeyer, previous contributors to this topic.
Disclosures
RE and MH declare that they have no competing interests.
Peer reviewers
Yosra Tahir Jarjees, MD
Assistant Professor
Head of Department of Obstetrics and Gynecology
Mosul College of Medicine
Mosul
Iraq
Disclosures
YTJ declares that he has no competing interests.
John Bachman, MD
Consultant in Family Medicine
Parker D Sanders and Isabella Sanders Professor of Primary Care
Rochester
MN
Disclosures
JB declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Jain V, Bos H, Bujold E; Society of Obstetricians and Gynaecologists of Canada. Guideline no. 402: diagnosis and management of placenta previa. J Obstet Gynaecol Can. 2020 Jul;42(7):906-17.e1. Abstract
Royal College of Obstetricians and Gynaecologists. Placenta praevia and placenta accreta: diagnosis and management. Green-top guideline no. 27a. Sep 2018 [internet publication].Full text
American College of Obstetricians and Gynecologists / Society for Maternal-Fetal Medicine. ACOG SMFM obstetric care consensus #7: placenta accreta spectrum. Dec 2018 [internet publication].Full text
Shipp TD, Poder L, Feldstein VA, et al; Expert Panel on GYN and OB Imaging, American College of Radiology. ACR appropriateness criteria: second and third trimester vaginal bleeding. J Am Coll Radiol. 2020 Nov;17(11s):S497-504.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Normal labor
- Placental abruption
- Miscarriage
More DifferentialsGuidelines
- Guideline no. 402: diagnosis and management of placenta previa
- Guideline no. 402: diagnosis and management of placenta previa
More GuidelinesPatient information
Premature labor
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer
