Summary
Definition
History and exam
Key diagnostic factors
- progressive headache
- severe headache
- meningismus
- symptoms of hydrocephalus (impaired cognitive function, confusion, coordination and gait disturbances, and urinary incontinence)
- behavioral or personality change
- reduced visual acuity and papilledema
Other diagnostic factors
- nausea or vomiting
- fever
- reduced conscious level
- cranial nerve palsies
- seizures
- weight loss
- mouth ulcers
- focal neurologic signs
- lymphadenopathy, hepatosplenomegaly
- dyspnea
- papular umbilicated skin lesions
- retinal defects
- nasal or palatal eschar
Risk factors
- HIV infection
- corticosteroid use
- underlying chronic disease (e.g., malignancy, organ failure, autoimmune disease, organ transplant)
- residing in or visiting northern Australia, Papua New Guinea, or Vancouver Island, Canada
- exposure to disturbed soil, chicken guano, or bat caves
- impaired cell-mediated immunity
- Filipinos and African Americans
- neutropenia or impaired phagocytic function
- neurosurgery
- infants and neonates
- central vascular catheters
- sinonasal disease
- antibacterial use
- prior surgery
- hyperalimentation
- intravenous drug use
Diagnostic tests
1st tests to order
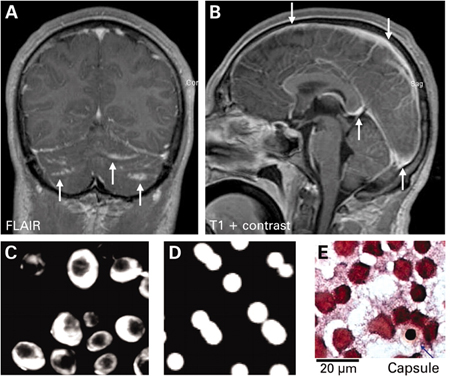
- CT and/or MRI head scan
- fungal blood cultures (3 sets)
- serum cryptococcal antigen test
- serum + urine Histoplasma antigen
- immunodiffusion tests (IgM and IgG) and complement fixation test (IgG) for coccidioidomycosis
- cerebrospinal fluid opening pressure
- cerebrospinal fluid (CSF) WBC and differential
- cerebrospinal fluid (CSF) protein
- cerebrospinal fluid (CSF) glucose
- cerebrospinal fluid India ink stain
- cerebrospinal fluid (CSF) culture
- cerebrospinal fluid cryptococcal polysaccharide antigen test
- cerebrospinal fluid Histoplasma antigen
- cerebrospinal fluid Histoplasma antibodies
- cerebrospinal fluid coccidioidal IgG antibodies
- cerebrospinal fluid (CSF) galactomannan antigen test
Tests to consider
- histopathology and culture of biopsies: meningeal, brain, extraneural sites of involvement
- polymerase chain reaction (PCR)
Emerging tests
- 18F-fluorodeoxyglucose (FDG) PET/CT
- cerebrospinal fluid (CSF) (1-3)-beta-D-glucan
Treatment algorithm
cryptococcal meningitis
histoplasmal meningitis
coccidioidal meningitis
candidal meningitis
Exserohilum rostratum meningitis
Aspergillus meningitis
mucormycosal meningitis
Contributors
Authors
Abhijit Chaudhuri, DM, MD, PhD, FACP, FRCP (Glasg), FRCP (Lond)
Consultant Neurologist
Clinical Lead of Neuroinflammation
Department of Neurology
Queen's Hospital
Romford
UK
Disclosures
AC declares that he has no competing interests.
Acknowledgements
Dr Abhijit Chaudhuri would like to gratefully acknowledge Dr Thomas S. Harrison and Dr Angela Loyse, previous contributors to this topic.
Disclosures
TSH and AL declare that they have no competing interests.
Peer reviewers
Robert A. Larsen, MD
Associate Professor of Medicine
University of Southern California
Keck School of Medicine
Los Angeles
CA
Disclosures
RAL declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Johnson RH, Einstein HE. Coccidioidal meningitis. Clin Infect Dis. 2006 Jan 1;42(1):103-7.Full text Abstract
World Health Organization. Guidelines for diagnosing, preventing and managing cryptococcal disease among adults, adolescents and children living with HIV. June 2022 [internet publication].Full text Abstract
National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association of the Infectious Disease Society of America. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Jul 2025 [internet publication].Full text
Galgiani JN, Ampel NM, Blair JE, et al. 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016 Sep 15;63(6):e112-46.Full text Abstract
Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016 Feb 15;62(4):e1-50.Full text Abstract
Patterson TF, Thompson GR 3rd, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016 Aug 15;63(4):e1-60.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Tuberculous meningitis
- Bacterial meningitis
- Viral meningitis
More DifferentialsGuidelines
- Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV
- Guidelines for diagnosing, preventing, and managing cryptococcal disease among adults, adolescents and children living with HIV
More GuidelinesPatient information
Lumbar puncture
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer