Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- coronary artery disease
- tachycardia
- hypotension
Outros fatores diagnósticos
- weak pulse
- syncope
- presyncope
- airway compromise
- impaired consciousness
- lightheadedness
- dizziness
- diminished responsiveness
- chest discomfort
- dyspnea
- asymptomatic
Fatores de risco
- coronary artery disease
- acute myocardial infarction
- left ventricular systolic dysfunction
- hypertrophic cardiomyopathy
- long QT syndrome
- short QT syndrome
- Brugada syndrome
- sleep-disordered breathing (SDB)
- family history of sudden death
- mental or physical stress
- ventricular pre-excitation
- arrhythmogenic right ventricular cardiomyopathy
- electrolyte imbalance
- drug toxicity
- Chagas disease and other cardiomyopathies
Investigações diagnósticas
Primeiras investigações a serem solicitadas
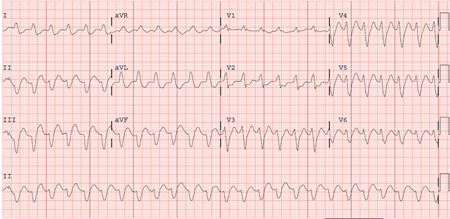
- ECG
- transthoracic echocardiogram
- electrolytes
- troponin I
Investigações a serem consideradas
- cardiac catheterization
- cardiac MRI
- electrophysiologic (EP) study
- genetic testing
Algoritmo de tratamento
hemodynamically unstable ventricular tachycardia with a pulse
torsades de pointes
catecholaminergic polymorphic ventricular tachycardia
hemodynamically stable nonidiopathic sustained ventricular tachycardia
hemodynamically stable idiopathic sustained ventricular tachycardia
nonidiopathic: at high risk for ventricular tachycardia or history of sustained ventricular tachycardia/cardiac arrest without identifiable reversible cause
idiopathic ventricular tachycardia
Colaboradores
Autores
Sei Iwai, MD, FACC, FHRS
Professor of Clinical Medicine
New York Medical College
Section Chief, Cardiac Electrophysiology
Westchester Medical Center Health Network
Valhalla
NY
Declarações
SI is an author of some references cited in this topic.
Agradecimentos
Professor Sei Iwai would like to gratefully acknowledge Dr Kenneth Stein and Dr Richard Keating, previous contributors to this topic.
Declarações
KS declares he is an employee of and shareholder in Boston Scientific, a manufacturer of implantable cardioverter defibrillators and ablation catheters. RK declares that he has no competing interests.
Revisores
Suneet Mittal, MD
Director
Electrophysiology Laboratory
The St. Luke's-Roosevelt Hospital Center
New York
NY
Declarações
SM declares that he has no competing interests.
Kenneth A. Ellenbogen, MD
Kontos Professor of Cardiology
Medical College of Virginia
Richmond
VA
Declarações
KAE declares that he has no competing interests.
Kim Rajappan, MA, MD, MRCP
Consultant Cardiologist and Electrophysiologist
Cardiac Department
John Radcliffe Hospital
Oxford
UK
Declarações
KR declares that she has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.Texto completo Resumo
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018 Oct 2;72(14):e91-220. Resumo
Pedersen CT, Kay GN, Kalman J, et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Heart Rhythm. 2014 Oct;11(10):e166-96.Texto completo Resumo
Panchal AR, Bartos JA, Cabañas JG, et al; Adult Basic and Advanced Life Support Writing Group. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 20;142(16_suppl_2):S366-468.Texto completo Resumo
Cronin EM, Bogun FM, Maury P, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. J Arrhythm. 2019 May 10;35(3):323-484.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Supraventricular tachycardia with aberrancy
- Supraventricular tachycardia with preexcitation
- Electrical artifact
Mais Diagnósticos diferenciaisDiretrizes
- 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy
- 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal
