Резюме
Определение
Анамнез и осмотр
Ключевые диагностические факторы
- coronary artery disease
- tachycardia
- hypotension
Другие диагностические факторы
- weak pulse
- syncope
- presyncope
- airway compromise
- impaired consciousness
- lightheadedness
- dizziness
- diminished responsiveness
- chest discomfort
- dyspnea
- asymptomatic
Факторы риска
- coronary artery disease
- acute myocardial infarction
- left ventricular systolic dysfunction
- hypertrophic cardiomyopathy
- long QT syndrome
- short QT syndrome
- Brugada syndrome
- sleep-disordered breathing (SDB)
- family history of sudden death
- mental or physical stress
- ventricular pre-excitation
- arrhythmogenic right ventricular cardiomyopathy
- electrolyte imbalance
- drug toxicity
- Chagas disease and other cardiomyopathies
Диагностические исследования
Исследования, которые показаны в первую очередь
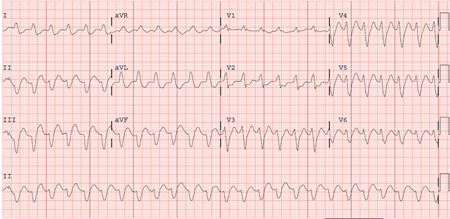
- ECG
- transthoracic echocardiogram
- electrolytes
- troponin I
Исследования, проведение которых нужно рассмотреть
- cardiac catheterization
- cardiac MRI
- electrophysiologic (EP) study
- genetic testing
Алгоритм лечения
hemodynamically unstable ventricular tachycardia with a pulse
torsades de pointes
catecholaminergic polymorphic ventricular tachycardia
hemodynamically stable nonidiopathic sustained ventricular tachycardia
hemodynamically stable idiopathic sustained ventricular tachycardia
nonidiopathic: at high risk for ventricular tachycardia or history of sustained ventricular tachycardia/cardiac arrest without identifiable reversible cause
idiopathic ventricular tachycardia
Составители
Авторы
Sei Iwai, MD, FACC, FHRS
Professor of Clinical Medicine
New York Medical College
Section Chief, Cardiac Electrophysiology
Westchester Medical Center Health Network
Valhalla
NY
Раскрытие информации
SI is an author of some references cited in this topic.
Выражение благодарностей
Professor Sei Iwai would like to gratefully acknowledge Dr Kenneth Stein and Dr Richard Keating, previous contributors to this topic.
Раскрытие информации
KS declares he is an employee of and shareholder in Boston Scientific, a manufacturer of implantable cardioverter defibrillators and ablation catheters. RK declares that he has no competing interests.
Рецензенты
Suneet Mittal, MD
Director
Electrophysiology Laboratory
The St. Luke's-Roosevelt Hospital Center
New York
NY
Раскрытие информации
SM declares that he has no competing interests.
Kenneth A. Ellenbogen, MD
Kontos Professor of Cardiology
Medical College of Virginia
Richmond
VA
Раскрытие информации
KAE declares that he has no competing interests.
Kim Rajappan, MA, MD, MRCP
Consultant Cardiologist and Electrophysiologist
Cardiac Department
John Radcliffe Hospital
Oxford
UK
利益声明
KR declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
参考文献
关键文献
Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.全文 摘要
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018 Oct 2;72(14):e91-220. 摘要
Pedersen CT, Kay GN, Kalman J, et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Heart Rhythm. 2014 Oct;11(10):e166-96.全文 摘要
Panchal AR, Bartos JA, Cabañas JG, et al; Adult Basic and Advanced Life Support Writing Group. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 20;142(16_suppl_2):S366-468.全文 摘要
Cronin EM, Bogun FM, Maury P, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. J Arrhythm. 2019 May 10;35(3):323-484.全文 摘要
参考文献
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
鉴别诊断
- Supraventricular tachycardia with aberrancy
- Supraventricular tachycardia with preexcitation
- Electrical artifact
更多 鉴别诊断指南
- 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy
- 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy
更多 指南登录或订阅即可浏览 BMJ Best Practice 临床实践完整内容
内容使用需遵循免责声明
