Evaluation of traumatic brain injury, acute
- Overview
- Theory
- Emergencies
- Diagnosis
- Resources
Summary
Definitions
Traumatic brain injury (TBI) is an acquired disruption of the normal function or structure of the brain caused by a head impact or external force.[1]McGinn MJ, Povlishock JT. Pathophysiology of traumatic brain injury. Neurosurg Clin N Am. 2016 Oct;27(4):397-407. http://www.ncbi.nlm.nih.gov/pubmed/27637392?tool=bestpractice.com [2]Centers for Disease Control and Prevention. Surveillance report of traumatic brain injury-related deaths by age group, sex, and mechanism of injury - United States, 2018 and 2019. 2022 [internet publication]. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-surveillance-report-2018-2019-508.pdf Blunt trauma, penetrating injuries, and blast injuries may cause TBI. However, not all impacts to the head cause TBI. Similar impacts in different people can lead to different injuries based on individual patient factors.
TBI is extremely heterogeneous, with short and long-term outcomes affected by the specific intracranial injury, concomitant extracranial injury, age, and pre-existing comorbidities.
Classification
TBI can be classified in numerous ways, including type, severity, location, mechanism of injury, and physiological response to injury.
Most classification systems are based on patient symptomatology, clinical exam or diagnostic findings during the early stabilization phase, which does not account for the evolving TBI process.
Both the Centers for Disease Control and Prevention and the World Health Organization agree that mild TBI is due to a blunt or mechanical force that results in some type of transient confusion, disorientation, or loss of consciousness lasting not more than 30 minutes; is possibly associated with transient neurobehavioral deficits; and has a Glasgow Coma Scale (GCS) score no lower than 13.[3]McCrea HJ, Perrine K, Niogi S, et al. Concussion in sports. Sports Health. 2013 Mar;5(2):160-4. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3658375 http://www.ncbi.nlm.nih.gov/pubmed/24427385?tool=bestpractice.com CDC: heads up Opens in new window This definition does not, however, identify all patients with significant intracranial injury as, although rare, some patients may present initially with none of these TBI symptoms.[4]Mower WR, Gupta M, Rodriguez R, et al. Validation of the sensitivity of the National Emergency X-Radiography Utilization Study (NEXUS) Head computed tomographic (CT) decision instrument for selective imaging of blunt head injury patients: an observational study. PLoS Med. 2017 Jul;14(7):e1002313. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002313 http://www.ncbi.nlm.nih.gov/pubmed/28700585?tool=bestpractice.com These "missed" patients become symptomatic over time, and so it has been suggested that classification based on repeated risk assessment over time would allow for the many variables that affect outcome.[5]Tenovuo O, Diaz-Arrastia R, Goldstein LE, et al. Assessing the severity of traumatic brain injury - time for a change? J Clin Med. 2021 Jan 4;10(1):148. https://www.mdpi.com/2077-0383/10/1/148 http://www.ncbi.nlm.nih.gov/pubmed/33406786?tool=bestpractice.com
Classification by clinical severity
TBI can be classified as mild, moderate, or severe, based on neurobehavioral deficits and advanced imaging findings after the injury. The term "concussion" is often used interchangeably with mild TBI.
The GCS is widely used to assess objectively the level of consciousness, and can range from 3 (completely unresponsive) to 15 (responsive). The GCS has been used extensively to classify TBI into levels of severity and prognosis.[6]Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017 Jan 1;80(1):6-15. https://braintrauma.org/uploads/03/12/Guidelines_for_Management_of_Severe_TBI_4th_Edition.pdf http://www.ncbi.nlm.nih.gov/pubmed/27654000?tool=bestpractice.com [7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com In the setting of TBI, there is a well-documented inverse relationship between the GCS and the incidence of positive findings on computed tomography (CT); the rate of intracranial injury and need for neurosurgical intervention doubles when the GCS drops from 15 to 14.[8]Smits M, Dippel DW, Steyerberg EW, et al. Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: the CHIP prediction rule. Ann Intern Med. 2007 Mar 20;146(6):397-405. http://www.ncbi.nlm.nih.gov/pubmed/17371884?tool=bestpractice.com [9]Ibañez J, Arikan F, Pedraza S, et al. Reliability of clinical guidelines in the detection of patients at risk following mild head injury: results of a prospective study. J Neurosurg. 2004 May;100(5):825-34. http://www.ncbi.nlm.nih.gov/pubmed/15137601?tool=bestpractice.com
Mild TBI: GCS 13-15; mortality 0.1%
Moderate TBI: GCS 9-12; mortality 10%
Severe TBI: GCS <9; mortality 40%.
There is continued controversy about including a GCS of 13 in the category of mild TBI, due to the higher incidence of intracranial injury in these patients compared with those with a GCS of 14 or 15.[10]Türedi S, Hasanbasoglu A, Gunduz A, et al. Clinical decision instruments for CT scan in minor head trauma. J Emerg Med. 2008 Apr;34(3):253-9. http://www.ncbi.nlm.nih.gov/pubmed/18180129?tool=bestpractice.com [11]Pearson WS, Ovalle F Jr, Faul M, et al. A review of traumatic brain injury trauma center visits meeting physiologic criteria from the american college of surgeons committee on trauma/centers for disease control and prevention field triage guidelines. Prehosp Emerg Care. 2012 Jul-Sep;16(3):323-8. http://www.ncbi.nlm.nih.gov/pubmed/22548387?tool=bestpractice.com [12]Mena JH, Sanchez AI, Rubiano AM, et al. Effect of the modified Glasgow Coma Scale score criteria for mild traumatic brain injury on mortality prediction: comparing classic and modified Glasgow Coma Scale score model scores of 13. J Trauma. 2011 Nov;71(5):1185-92;discussion 1193. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217203 http://www.ncbi.nlm.nih.gov/pubmed/22071923?tool=bestpractice.com Clinical guidelines in Australia recognize the increased morbidity associated with a GCS of 13, and limit the classification of mild TBI to those patients with a GCS of 14 or 15.[13]New South Wales Ministry of Health. Closed head injury in adults - initial management. Feb 2012 [internet publication]. http://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2012_013.pdf
The Mayo classification system for TBI classifies patients with TBI into definite, probable, and possible, based on the patient’s clinical and CT findings.[14]Malec JF, Brown AW, Leibson CL, et al. The Mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007 Sep;24(9):1417-24. http://www.ncbi.nlm.nih.gov/pubmed/17892404?tool=bestpractice.com
Classification by broad etiology
May be blunt, penetrating, or blast-related.
Blunt TBI: occurs when external mechanical force leads to rapid acceleration or deceleration with brain impact. Blunt TBI is typically found in the setting of motor vehicle-related injury, falls, crush injuries, or physical altercations.
Penetrating TBI: occurs when an object pierces the skull and breaches the dura mater, seen commonly in gunshot and stab wounds.
Blast TBI: commonly occurs after bombings and warfare, due to a combination of contact and inertial forces, overpressure, and acoustic waves.[15]Ling G, Bandak F, Armonda R, et al. Explosive blast neurotrauma. J Neurotrauma. 2009 Jun;26(6):815-25. http://www.ncbi.nlm.nih.gov/pubmed/19397423?tool=bestpractice.com
Classification by area of involvement
TBI can be classified by area of the brain involved, as in diffuse or focal, although the two types frequently coexist.[16]Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008 Aug;7(8):728-41. http://www.ncbi.nlm.nih.gov/pubmed/18635021?tool=bestpractice.com
Diffuse brain injury includes diffuse axonal injury, hypoxic brain injury, diffuse cerebral edema, or diffuse vascular injury.
Focal injury includes specific lesions such as contusions, intracranial hematomas, infarctions, axonal tears, cranial nerve avulsions, and skull fractures.
Classification by injury progression: primary versus secondary
Primary injury is due to the immediate mechanical force, whether blunt, penetrating, or blast, and may include the following:
Concussion: symptoms without intracranial injury detected on CT
Skull fracture
Contusion: localized punctate hemorrhages
Hematoma: subdural, epidural, intracerebral
Subarachnoid hemorrhage
Axonal shear or laceration.
Secondary injury refers to the evolving pathophysiological consequences of the primary injury and encompasses a multitude of complex neurobiological cascades altered or initiated at a cellular level following the primary injury, and may include the following:[16]Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008 Aug;7(8):728-41. http://www.ncbi.nlm.nih.gov/pubmed/18635021?tool=bestpractice.com
Cerebral edema
Increased intracranial pressure
Hemorrhage progression
Seizures
Ischemia
Infection
Traumatic venous sinus thrombosis.
Epidemiology
TBI is a substantial cause of morbidity and mortality; in the US, 60,611 TBI-related deaths occurred during 2019.[2]Centers for Disease Control and Prevention. Surveillance report of traumatic brain injury-related deaths by age group, sex, and mechanism of injury - United States, 2018 and 2019. 2022 [internet publication]. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-surveillance-report-2018-2019-508.pdf Annual TBI-related emergency department visits of approximately 2.5 million have been reported in the US.[17]Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017 Mar 17;66(9):1-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829835 http://www.ncbi.nlm.nih.gov/pubmed/28301451?tool=bestpractice.com In England and Wales, over 1 million people attend emergency departments each year with a recent head injury, and approximately 40,000 of those admitted have evidence of TBI.[18]National Institute for Health and Care Excellence (UK). Head injury: assessment and early management. May 2023 [internet publication]. https://www.nice.org.uk/guidance/ng232 The burden of disability and death due to TBI is higher in low- and middle-income countries compared with high-income countries.[19]Maas AIR, Menon DK, Adelson PD, et al; InTBIR Participants and Investigators. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017 Dec;16(12):987-1048. http://www.ncbi.nlm.nih.gov/pubmed/29122524?tool=bestpractice.com
Approximately 80% to 90% of patients with TBI are treated and released without hospital admission.[20]Kay A, Teasdale G. Head injury in the United Kingdom. World J Surg. 2001 Sep;25(9):1210-20. http://www.ncbi.nlm.nih.gov/pubmed/11571960?tool=bestpractice.com [21]Centers for Disease Control and Prevention. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002-2006 (Blue Book). Mar 2010 [internet publication]. https://www.cdc.gov/traumaticbraininjury/tbi_ed.html
TBI most frequently occurs in very young children (ages 0 to 4 years), and in adolescence and young adulthood (ages 15 to 24 years), with a subsequent peak in incidence in older adults (over age 65).[17]Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017 Mar 17;66(9):1-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829835 http://www.ncbi.nlm.nih.gov/pubmed/28301451?tool=bestpractice.com Older age comprises the group with the highest rates of TBI-related hospitalizations and deaths.[2]Centers for Disease Control and Prevention. Surveillance report of traumatic brain injury-related deaths by age group, sex, and mechanism of injury - United States, 2018 and 2019. 2022 [internet publication]. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-surveillance-report-2018-2019-508.pdf [17]Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017 Mar 17;66(9):1-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829835 http://www.ncbi.nlm.nih.gov/pubmed/28301451?tool=bestpractice.com
Estimated average annual rates of TBI are higher for males than for females across all age groups.[17]Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017 Mar 17;66(9):1-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829835 http://www.ncbi.nlm.nih.gov/pubmed/28301451?tool=bestpractice.com The age-adjusted rate of TBI-related deaths per 100,000 population in males (26.8 in 2018 and 26.6 in 2019) was more than three times the rate of females (8.2 in 2018 and 8.1 in 2019).[2]Centers for Disease Control and Prevention. Surveillance report of traumatic brain injury-related deaths by age group, sex, and mechanism of injury - United States, 2018 and 2019. 2022 [internet publication]. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-surveillance-report-2018-2019-508.pdf
Concussion and post-concussive symptoms
Concussion symptoms include short-lived confusion, disorientation, or loss of consciousness, with or without neurobehavioral deficits. Concussion symptoms occur in most patients with TBI, and are typically the only finding in patients with mild TBI. Patients with moderate or severe TBI typically have more severe neurocognitive deficits that overshadow the concussive symptoms.
The five major subtypes of concussion include headache, cognitive, vestibular, mood, and ocular-motor. One meta-analysis demonstrated that headache and cognitive symptoms are the most common subtypes in both adults and children.[22]Lumba-Brown A, Teramoto M, Bloom OJ, et al. Concussion guidelines step 2: Evidence for subtype classification. Neurosurgery. 2020 Jan 1;86(1):2-13. https://www.doi.org/10.1093/neuros/nyz332 http://www.ncbi.nlm.nih.gov/pubmed/31432081?tool=bestpractice.com
The World Health Organization’s definition of post-concussive syndrome includes the presence of 3 or more of the following symptoms after a head injury: headache, dizziness, fatigue, irritability, difficulty with concentrating and performing mental tasks, impairment of memory, insomnia and reduced tolerance to stress, emotional excitement, or alcohol.[23]World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. 1992 [internet publication]. https://apps.who.int/iris/handle/10665/37958
In 2017, 15% of high school students in the US reported at least one sports-related concussion in the past year.[24]DePadilla L, Miller GF, Jones SE, et al. Self-reported concussions from playing a sport or being physically active among high school students - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018 Jun 22;67(24):682-5. https://www.cdc.gov/mmwr/volumes/67/wr/mm6724a3.htm?s_cid=mm6724a3_w http://www.ncbi.nlm.nih.gov/pubmed/29927909?tool=bestpractice.com Approximately 30% of children and adults experience persistent post-concussive symptoms lasting more than 30 days after injury.[25]Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016 Mar 8;315(10):1014-25. http://www.ncbi.nlm.nih.gov/pubmed/26954410?tool=bestpractice.com [26]de Koning ME, Scheenen ME, van der Horn HJ, et al. Non-hospitalized patients with mild traumatic brain injury: the forgotten minority. J Neurotrauma. 2017 Jan 1;34(1):257-61. http://www.ncbi.nlm.nih.gov/pubmed/27029852?tool=bestpractice.com
Hemorrhage
Subarachnoid hemorrhage (SAH) is one of the most common CT findings in TBI, occurring in about 30% to 40% of patients with moderate to severe TBI, and 5% of patients with mild TBI.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com [27]Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008 Aug 5;5(8):e165. http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0050165 http://www.ncbi.nlm.nih.gov/pubmed/18684008?tool=bestpractice.com [28]Roberts I, Yates D, Sandercock P, et al; CRASH trial collaborators. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004 Oct 9-15;364(9442):1321-8. http://www.ncbi.nlm.nih.gov/pubmed/15474134?tool=bestpractice.com SAH is frequently associated with other intracranial injuries. SAH is associated with a poorer outcome in patients with moderate or severe TBI, although it is unclear whether the SAH is simply a marker of severity of injury, or if the poorer outcomes are due to subsequent vasospasm.[29]Kramer DR, Winer JL, Pease BA, et al. Cerebral vasospasm in traumatic brain injury. Neurol Res Int. 2013;2013:415813. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3703898 http://www.ncbi.nlm.nih.gov/pubmed/23862062?tool=bestpractice.com
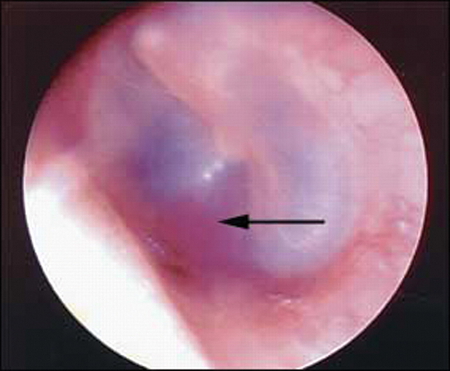
Subdural hematomas (SDH) are the most common type of mass lesion in TBI, seen in about 20% of patients with moderate to severe TBI, and in about 30% of fatal TBI. SDH occur in only 3% of patients with mild TBI. SDH that lead to hospitalizations or deaths are most commonly secondary to motor vehicle-related injury in younger adults, and falls in older adults.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com [30]Bullock MR, Chesnut R, Ghajar J, et al; Surgical Management of Traumatic Brain Injury Author Group. Surgical management of acute subdural hematomas. Neurosurgery. 2006 Mar;58(3 suppl):S16-24. http://www.ncbi.nlm.nih.gov/pubmed/16710968?tool=bestpractice.com [31]Urban JE, Whitlow CT, Edgerton CA, et al. Motor vehicle crash-related subdural hematoma from real-world head impact data. J Neurotrauma. 2012 Dec 10;29(18):2774-81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521134 http://www.ncbi.nlm.nih.gov/pubmed/22928543?tool=bestpractice.com
Epidural hematoma (EDH) is seen in about 10% of patients with moderate to severe TBI and about 1% of patients with mild TBI. The incidence of EDH is highest among adolescents and young adults, most commonly between 20 and 30 years of age. Most cases of EDH are caused by traffic accidents, falls, and assaults.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com [27]Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008 Aug 5;5(8):e165. http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0050165 http://www.ncbi.nlm.nih.gov/pubmed/18684008?tool=bestpractice.com
Intracerebral hematomas occur in 10% to 30% of patients with moderate to severe TBI, and <1% of patients with mild TBI.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com [16]Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008 Aug;7(8):728-41. http://www.ncbi.nlm.nih.gov/pubmed/18635021?tool=bestpractice.com
Cerebral contusions
Occur in 20% to 30% of patients with moderate to severe TBI, and 6% of patients with mild TBI.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com [28]Roberts I, Yates D, Sandercock P, et al; CRASH trial collaborators. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004 Oct 9-15;364(9442):1321-8. http://www.ncbi.nlm.nih.gov/pubmed/15474134?tool=bestpractice.com [32]Iaccarino C, Schiavi P, Picetti E, et al. Patients with brain contusions: predictors of outcome and relationship between radiological and clinical evolution. J Neurosurg. 2014 Apr;120(4):908-18. http://www.ncbi.nlm.nih.gov/pubmed/24506250?tool=bestpractice.com
Axonal injury
Probably present in a majority of patients with TBI to some degree, although low-grade axonal injury is microscopic and not detected by CT.
Diffuse axonal injury (DAI) is thought to be present to some degree in all TBI-related fatalities and those resulting in a persistent vegetative state. The presence of DAI increases the likelihood of a poor outcome.[33]van Eijck MM, Schoonman GG, van der Naalt J, et al. Diffuse axonal injury after traumatic brain injury is a prognostic factor for functional outcome: a systematic review and meta-analysis. Brain Inj. 2018;32(4):395-402. http://www.ncbi.nlm.nih.gov/pubmed/29381396?tool=bestpractice.com The initial CT is normal in 50% to 80% of patients ultimately diagnosed with DAI, but magnetic resonance imaging shows evidence of axonal injury in 70% of patients with moderate to severe TBI.[34]Skandsen T, Kvistad KA, Solheim O, et al. Prevalence and impact of diffuse axonal injury in patients with moderate and severe head injury: a cohort study of early magnetic resonance imaging findings and 1-year outcome. J Neurosurg. 2010 Sep;113(3):556-63. http://www.ncbi.nlm.nih.gov/pubmed/19852541?tool=bestpractice.com
Skull fractures
Occur in about 5% of patients with mild TBI and up to 50% of those with severe TBI. Most skull fractures are due to falls, assaults, or motor vehicle-related injuries. The most common fractures are simple linear fractures, comprising >50% of all skull fractures. Less than 1% of patients with mild TBI have a depressed skull fracture.[7]Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001 May 5;357(9266):1391-6. http://www.ncbi.nlm.nih.gov/pubmed/11356436?tool=bestpractice.com
Penetrating or blast injury
Penetrating injuries are classified as high- or low-velocity, and may be self-inflicted, non-intentional, or related to an assault. A single gunshot wound to the head has 50% mortality.[35]Cripps MW, Ereso AQ, Sadjadi J, et al. The number of gunshot wounds does not predict injury severity and mortality. Am Surg. 2009 Jan;75(1):44-8. http://www.ncbi.nlm.nih.gov/pubmed/19213396?tool=bestpractice.com
Blast injuries are a leading cause of TBI in active duty military personnel in war zones, accounting for about 60% of all severe TBI.[36]DuBose JJ, Barmparas G, Inaba K, et al. Isolated severe traumatic brain injuries sustained during combat operations: demographics, mortality outcomes, and lessons to be learned from contrasts to civilian counterparts. J Trauma. 2011 Jan;70(1):11-8. http://www.ncbi.nlm.nih.gov/pubmed/21217475?tool=bestpractice.com [37]Ling G, Ecklund JM, Bandak FA. Brain injury from explosive blast: description and clinical management. Handb Clin Neurol. 2015;127:173-80. http://www.ncbi.nlm.nih.gov/pubmed/25702216?tool=bestpractice.com
Differentials
Common
- Skull fracture (nonbasilar)
- Base of skull fracture
- Cerebral contusion
- Intracerebral hemorrhage
- Subdural hematoma
- Epidural hematoma
- Intraventricular hemorrhage
- Traumatic subarachnoid hemorrhage
- Penetrating injuries
- Diffuse axonal injury
- Mild traumatic brain injury
Contributors
Authors
Micelle J. Haydel, MD
Albert J. Lauro Professor of Medicine/Emergency Medicine
Clinical Professor Medicine/Emergency Medicine
Section of Emergency Medicine
Louisiana State University Health Science Center
New Orleans
LA
Disclosures
MJH is an author of a reference cited in this topic.
Acknowledgements
Dr Micelle J. Haydel would like to gratefully acknowledge Dr Victoria E. Johnson, Dr Marek Ma, Dr Nathan Ranalli, and Dr Douglas H. Smith, previous contributors to this topic.
Disclosures
VEJ, MM, NR, and DHS declare that they have no competing interests.
Peer reviewers
David W. Wright, MD
Director of Research
Department of Emergency Medicine
Emory University
Atlanta
GA
Disclosures
DWW declares that he has no competing interests.
David Sharp, MBBS, BA, MRCP, PhD
Senior Lecturer In Neurology
Imperial College
London
UK
Divulgaciones
DS declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017 Jan 1;80(1):6-15.Texto completo Resumen
National Institute for Health and Care Excellence (UK). Head injury: assessment and early management. May 2023 [internet publication].Texto completo
Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the Brain Trauma Foundation guidelines. Pediatr Crit Care Med. 2019 Mar;20(3s suppl 1):S1-82.Texto completo Resumen
Expert Panel on Neurological Imaging; Shih RY, Burns J, Ajam AA. ACR Appropriateness Criteria® head trauma: 2021 update. J Am Coll Radiol. 2021 May;18(5S):S13-36.Texto completo Resumen
Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018 Nov 1;172(11):e182853.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Calculadoras
Glasgow Coma Scale
Canadian Head CT Rule for Minor Head Injury
Más CalculadorasVideos
Venepuncture and phlebotomy: animated demonstration
Más vídeosInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad