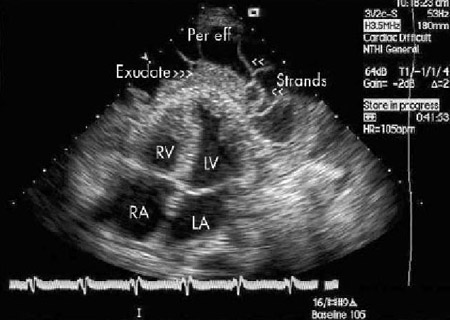
Pericardial effusion is present when the fluid in the pericardial space exceeds its physiologic amount (≤50 mL). In the clinical setting, pericardial effusion is relatively common. It may be detected incidentally on a cardiac or chest imaging study, or manifest on the background of a cardiac or systemic disease.
The significance of effusions lies in their relationship to an underlying disease state and in their potential to affect a patient's hemodynamics.
Epidemiology
Data from the Framingham cohort suggest that pericardial effusion may be present in up to 6.5% of the general adult population.[1]Savage DD, Garrison RJ, Brand F, et al. Prevalence and correlates of posterior extra echocardiographic spaces in a free-living population based sample (the Framingham study). Am J Cardio. 1983;51:1207-12.
http://www.ncbi.nlm.nih.gov/pubmed/6220597?tool=bestpractice.com
Prevalence increased with age, from <1% in patients ages 20 to 30 years to more than 15% in patients ages 80 years and over. Most people in the study had small effusions and no recognizable cardiac disease.[1]Savage DD, Garrison RJ, Brand F, et al. Prevalence and correlates of posterior extra echocardiographic spaces in a free-living population based sample (the Framingham study). Am J Cardio. 1983;51:1207-12.
http://www.ncbi.nlm.nih.gov/pubmed/6220597?tool=bestpractice.com
In the clinical setting, the prevalence of pericardial effusion depends on the patient population studied. Over a 6-year period, the mean annual prevalence and incidence of pericardial effusion in an echocardiography laboratory of a large Italian hospital was 3% and 9%, respectively.[2]Imazio M, Mayosi BM, Brucato A, et al. Triage and management of pericardial effusion. J Cardiovasc Med (Hagerstown). 2010 Dec;11(12):928-35.
http://www.ncbi.nlm.nih.gov/pubmed/20814314?tool=bestpractice.com
In high-risk emergency department patients, the prevalence of pericardial effusion has been reported in the range of 13% to 20%.[3]Arntfield RT, Millington SJ. Point of care cardiac ultrasound applications in the emergency department and intensive care unit - a review. Curr Cardiol Rev. 2012 May;8(2):98-108.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3406278
http://www.ncbi.nlm.nih.gov/pubmed/22894759?tool=bestpractice.com
One meta-analysis reported pooled pericardial effusion prevalence of 19.5% across studies that included patients with pulmonary arterial hypertension, chronic heart failure, myocardial infarction, and malignancy.[4]De Filippo O, Gatti P, Rettegno S, et al. Is pericardial effusion a negative prognostic marker? Meta-analysis of outcomes of pericardial effusion. J Cardiovasc Med (Hagerstown). 2019 Jan;20(1):39-45.
http://www.ncbi.nlm.nih.gov/pubmed/30480582?tool=bestpractice.com
Pericardial anatomy and physiology
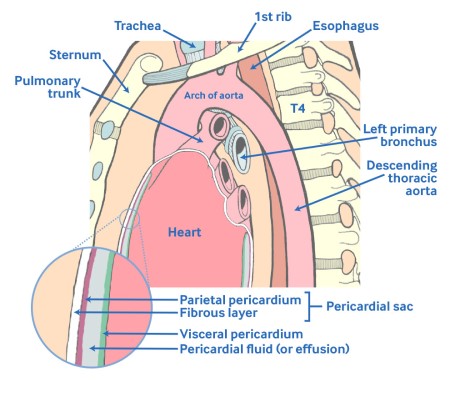
The normal pericardium consists of both fibrous and serous components. The fibrous layer forms a sac that contains the heart and the roots of the great vessels. The serous part is further divided into a layer that is adherent to the heart and epicardial fat (epicardium or visceral pericardium) and a layer that lines the internal surface of the fibrous layer (parietal pericardium). The pericardial space enclosed between the visceral and the parietal pericardium normally contains up to 50 mL of serous fluid. A pericardial effusion is present when accumulated fluid in the pericardial space exceeds this physiologic amount.[5]Hoit BD. Pericardial effusion and cardiac tamponade in the new millennium. Curr Cardiol Rep. 2017 Jul;19(7):57.
http://www.ncbi.nlm.nih.gov/pubmed/28493085?tool=bestpractice.com
The pericardium serves as a protective barrier, promotes efficient cardiac function, and prohibits excessive displacement of the heart.
Under normal conditions, a pericardial reserve volume exists to accommodate physiologic changes in ventricular filling conditions. However, if this reserve volume is exceeded, pericardial pressure increases rapidly and significantly limits cardiac filling. The relatively inelastic pericardium is able to stretch under conditions of chronic stress such as left ventricular dilation or a slowly accumulating pericardial effusion. However, once the pericardial pressure-volume relationship reaches its noncompliant stage, expansion is limited and small increases in volume produce a dramatic increase in pericardial pressure, severely impairing ventricular filling.[Figure caption and citation for the preceding image starts]: Diagram showing the anatomy of the pericardium.Marchand P. Thorax. 1951;6:359-368 [Citation ends].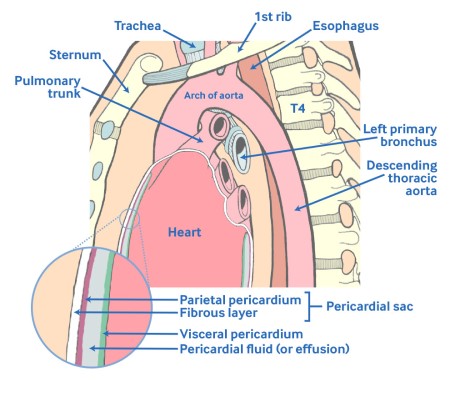
Classification of pericardial effusion
Pericardial effusion can be classified by:
Onset (acute or subacute vs. chronic [when lasting >3 months])
Distribution (circumferential or loculated)
Hemodynamic impact (cardiac tamponade or no cardiac tamponade)
Composition (serous fluid, blood, rarely air, or gas from bacterial infections)
Size based on a simple semiquantitative echocardiographic assessment.
The size of the effusion on echocardiography indicates the volume of pericardial fluid as follows:[5]Hoit BD. Pericardial effusion and cardiac tamponade in the new millennium. Curr Cardiol Rep. 2017 Jul;19(7):57.
http://www.ncbi.nlm.nih.gov/pubmed/28493085?tool=bestpractice.com
[6]Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines on the diagnosis and management of pericardial diseases. Eur Heart J. 2015;36:2921-64.
https://academic.oup.com/eurheartj/article/36/42/2921/2293375
http://www.ncbi.nlm.nih.gov/pubmed/26320112?tool=bestpractice.com
[7]Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013 Sep;26(9):965-1012.e15.
https://www.onlinejase.com/article/S0894-7317(13)00533-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23998693?tool=bestpractice.com
Trivial (seen only in systole)
Small (<10 mm), which corresponds to 50-100 mL pericardial fluid
Moderate (10-20 mm), corresponding to 100-500 mL pericardial fluid
Large (>20 mm), corresponding to >500 mL pericardial fluid
Very large (>25 mm); usually indicates >700 mL pericardial fluid.
The development of a pericardial effusion often has important implications for the diagnosis and/or prognosis of the underlying disease.[5]Hoit BD. Pericardial effusion and cardiac tamponade in the new millennium. Curr Cardiol Rep. 2017 Jul;19(7):57.
http://www.ncbi.nlm.nih.gov/pubmed/28493085?tool=bestpractice.com