Summary
Definition
History and exam
Key diagnostic factors
- abdominal pain
- prolonged diarrhea
- perianal lesions
Other diagnostic factors
- bowel obstruction
- blood in stools
- fatigue
- abdominal tenderness
- weight loss
- fever
- oral lesions
- abdominal mass
- extraintestinal manifestations (e.g., erythema nodosum or pyoderma gangrenosum)
Risk factors
- white ethnicity
- Ashkenazi Jewish ancestry
- age 15-40 or 50-60 years
- family history of CD
- use of antibiotics
- cigarette smoking
- diet high in refined sugar
- diet low in fiber
- diet high in ultra-processed foods
- use of oral contraceptives
- not breastfed
- use of nonsteroidal anti-inflammatory drugs (NSAIDs)
Diagnostic tests
1st tests to order
- CBC
- iron studies (serum iron, serum ferritin, total iron binding capacity [TIBC], transferrin saturation)
- serum vitamin B12
- serum folate
- comprehensive metabolic panel (CMP)
- CRP and erythrocyte sedimentation rate (ESR)
- stool testing
- Yersinia enterocolitica serology
- plain abdominal x-ray
- MRI abdomen/pelvis
- CT abdomen
Tests to consider
- abdominal and pelvic ultrasonography
- ileocolonoscopy
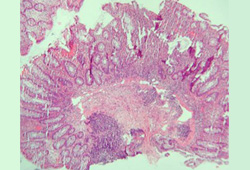
- tissue biopsy
- esophagogastroduodenoscopy
- wireless capsule endoscopy
- fecal calprotectin
Emerging tests
- serologic markers
Treatment algorithm
ileocecal disease not fistulizing with <100 cm of bowel affected: initial presentation or relapse
colonic disease not fistulizing: initial presentation or relapse
extensive small bowel disease (>100 cm of bowel affected) not fistulizing: initial presentation or relapse
upper gastrointestinal disease (esophageal and/or gastroduodenal disease) not fistulizing: initial presentation or relapse
perianal or fistulizing disease: initial presentation or relapse
in remission
Contributors
Authors
Lucy Charlotte Hicks, MBBS, PhD, FHEA, MRCP
Consultant Gastroenterologist
Department of Gastroenterology
St Mary's Hospital
Imperial College Healthcare NHS Trust
Honorary Senior Clinical Lecturer
Imperial College
London
UK
Disclosures
LCH has received costs for travel and accommodation from Takeda.
Georgia Woodfield, MBChB, MSc, PhD, MRCP
Consultant Gastroenterologist
Department of Gastroenterology
Royal Free Hospital
Royal Free London NHS Foundation Trust
London
UK
Disclosures
GW declares that she has no competing interests.
Acknowledgements
Dr Georgia Woodfield and Dr Lucy Charlotte Hicks would like to gratefully acknowledge Mr George Reese, Dr Pranav H. Patel, Dr Philip J. Smith, Dr Charlotte Ford, Dr Wissam Bleibel, Dr Bishal Mainali, Dr Chandrashekhar Thukral, and Dr Mark A. Peppercorn, the previous contributors to this topic.
Disclosures
GR is an author of a number of references cited in this topic. PHP, PJS, CF, WB, BM, CT, and MAP declare that they have no competing interests.
Peer reviewers
Kiron M. Das, MD, PhD, FACP, FRCP
Chief of Gastroenterology & Hepatology
Professor of Medicine
Director of Crohn's & Colitis Center of New Jersey
New Brunswick
NJ
Disclosures
KMD declares that he has no competing interests.
John Mansfield, MA, MD, FRCP
Consultant Gastroenterologist and Senior Lecturer
Royal Victoria Infirmary
Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University
Newcastle upon Tyne
UK
Disclosures
JM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific consensus statements on Crohn's disease. Part 1: definition, diagnosis, and epidemiology. J Gastroenterol Hepatol. 2016 Jan;31(1):45-55.Full text Abstract
Lichtenstein GR, Loftus EV, Isaacs KL, et al. ACG clinical guideline: management of Crohn's disease in adults. Am J Gastroenterol. 2018 Apr;113(4):481-517.Full text Abstract
Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn's disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017 Jan;11(1):3-25.Full text Abstract
Torres J, Bonovas S, Doherty G, et al. ECCO guidelines on therapeutics in Crohn's disease: medical treatment. J Crohns Colitis. 2020 Jan 1;14(1):4-22.Full text Abstract
Adamina M, Bonovas S, Raine T, et al. ECCO guidelines on therapeutics in Crohn's disease: surgical treatment. J Crohns Colitis. 2020 Feb 10;14(2):155-68.Full text Abstract
Feuerstein JD, Ho EY, Shmidt E, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021 Jun;160(7):2496-508.Full text Abstract
Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: surgical management and special situations. J Crohns Colitis. 2017 Feb;11(2):135-49.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Ulcerative colitis (UC)
- Infectious colitis
- Pseudomembranous colitis
More DifferentialsGuidelines
- BSG consensus guidelines on the management of inflammatory bowel disease in adults
- Management of Crohn's disease in adults
More GuidelinesPatient information
Crohn disease: what is it?
Crohn disease: what are the treatment options?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer