Definitions
Coma is the absence of consciousness.
This state of unarousable unconsciousness includes the failure of eye opening to stimulation, a motor response no better than simple withdrawal-type movements, and a verbal response no better than simple vocalization of nonword sounds. This presupposes that the motor pathways and systems that would allow a conscious patient to respond are intact.[1]Posner JB, Saper CB, Schiff ND, et al. Psychogenic unresponsiveness. Plum and Posner's diagnosis of stupor and coma. New York, NY: Oxford University Press; 2007.[2]Wijdicks EFM. The comatose patient. New York, NY: Oxford University Press; 2007.[3]Young GB, Wijdicks EFM, eds. Disorders of consciousness. Volume 90. The Handbook of Clinical Neurology, 3rd series. New York, NY: Elsevier; 2008.
Full consciousness is an awake state in which one is aware of oneself and the environment, including the ability to perceive and interpret stimuli and to interact and communicate with others in the absence of motor deficits.
Basic alerting and wakefulness is a function of the ascending reticular activating system (ARAS).
Awareness is more complex and incompletely understood. It has multiple hierarchies (the highest probably being self-awareness and apperception) and components (e.g., perception, memory, attention, language and other symbolic coding, emotion, motivation, response selection). These components of awareness, and full conscious awareness itself, are now thought to relate to the integrated action of networks of cerebral cortical regions.[4]Sporns O. Structure and function of complex brain networks. Dialogues Clin Neurosci. 2013 Sep;15(3):247-62.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3811098
http://www.ncbi.nlm.nih.gov/pubmed/24174898?tool=bestpractice.com
In the assessment of conscious awareness, the Coma Recovery Scale-Revised (CRS-R) is useful in grading and tracking the level of consciousness.[5]Bodien YG, Carlowicz CA, Chatelle C, et al. Sensitivity and specificity of the coma recovery scale--revised total score in detection of conscious awareness. Arch Phys Med Rehabil. 2016 Mar;97(3):490-492.e1.
http://www.ncbi.nlm.nih.gov/pubmed/26342571?tool=bestpractice.com
Brain death
The irreversible, total destruction of all brainstem functions, including the capacity for alertness, cranial nerve functions, and apnea (UK), or all brain function (whole brain death in US).
There are guidelines for the neurologic determination of death in infants, children, and adults.[6]Greer DM, Kirschen MP, Lewis A, et al. Pediatric and adult brain death/death by neurologic criteria consensus guideline. Neurology. 2023 Dec 12;101(24):1112-32.
https://www.neurology.org/doi/10.1212/WNL.0000000000207740
http://www.ncbi.nlm.nih.gov/pubmed/37821233?tool=bestpractice.com
Brain death must never be diagnosed without an etiology.
Vegetative state (unresponsive wakefulness syndrome [UWS])
The complete loss of awareness with preserved wakefulness and wake-sleep-cycles. Thalamocortical function is severely disrupted. VS is commonly due to severe cerebral cortical damage (usually by anoxia-ischemia after cardiac arrest or less commonly by hypoglycemia), by damage to the white matter of the cerebrum (most commonly related to diffuse axonal injury from traumatic brain injury), or thalamic damage (by anoxia-ischemia or structural lesions such as tumors or strokes). A new term, UWS, is gradually replacing VS as some patients who are behaviorally unresponsive may have “covert awareness”, as revealed by specialized testing such as functional magnetic resonance imaging (fMRI).[7]Laureys S, Celesia GG, Cohadon F, et al. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med. 2010 Nov 1;8:68.
https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-8-68
http://www.ncbi.nlm.nih.gov/pubmed/21040571?tool=bestpractice.com
Minimally conscious state (MCS)
Delirium
Neglect syndrome
Encephalopathy
Diffuse disturbance of cerebral function in the absence of overt parenchymal inflammation or structural abnormality.
There are numerous encephalopathies due to electrolyte disturbances, disturbances in thyroid function, inborn errors of metabolism (e.g., porphyria, mitochondrial disorders), organ failure (e.g., hepatic encephalopathy), systemic inflammation (e.g., due to burns), and cardiac arrest (anoxic-ischemic encephalopathy). Most of these cause reversible, functional dysfunction of the ARAS and cause a more diffuse disturbance without localizing signs.
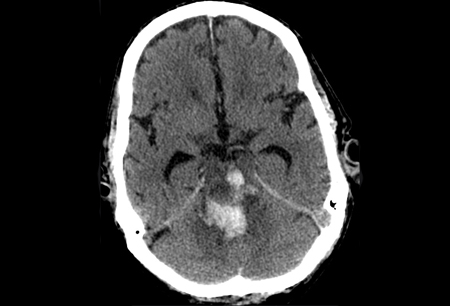
Mass lesion
Includes brain abscess, tumor, intracerebral hemorrhage, and trauma with epidural or subdural hematoma.
Depending on the case mix, mass lesions causing coma are common, especially in centers with patients with trauma, cancer, or stroke, and even in general hospitals.
It is important to recognize early phases of herniation syndromes (caused by shifts of brain structures from one compartment to another), and to investigate and treat before irreversible damage occurs. Consciousness is impaired due to compression of ARAS components.
In subfalcine herniation, the midline structures of the supratentorial space are laterally displaced, causing pressure on the thalamus and progressive impairment of consciousness with or without hemiparesis, and oculomotor palsy in later stages.
With transtentorial herniation there is downward displacement of the uncus (uncal herniation) or diencephalic structures (thalamus and hypothalamus) through the tentorial opening. This causes brainstem compression with early oculomotor palsy often before loss of consciousness.
Tonsillar herniation through the foramen magnum compresses the caudal medullary respiratory center, causing respiratory arrest and brain death.
Central (diencephalic) herniation is said to be common. Compression of the midbrain produces irreversible bilateral oculomotor palsies in later stages.
Rostrocaudal deterioration of brainstem function occurs with brainstem distortion affecting microvascular perfusion of tissue. Loss of consciousness is typically abrupt with cranial nerve palsies.
Disorders mimicking comas
Locked-in state is when consciousness is preserved but motor output is impaired (e.g., due to basis pontis lesions, severe polyneuropathies such as Guillain-Barre syndrome or pharmacologic paralysis).
Psychogenic unresponsiveness relates to lack of responsiveness due to psychogenic causes, in the absence of any toxic, metabolic, inflammatory, or structural damage to the brain (e.g., pseudocoma, pseudoseizure, psychogenic seizures).
Transient coma
Syncope (fainting) is a transient coma due to the temporary reduction of global brain perfusion, which can be due to cardiac etiologies, vasomotor etiologies, orthostatic hypotension, or pulmonary embolism.
Seizures produce transient coma due to epileptiform discharges in the brain, either as absence/petit mal seizures (bifrontal or diffuse cortical and thalamic involvement), focal unaware seizures (usually of temporal lobe origin, associated with diffuse limbic involvement and cerebral cortical inhibition), or generalized convulsive seizures (with seizure discharges involving both cerebral hemispheres and brainstem structures). Coma can be prolonged in status epilepticus (e.g., nonconvulsive status epilepticus as diagnosed by EEG). Convulsive movements and incontinence can occur, especially with generalized tonic-clonic seizures.
Concussion is the transient impairment of consciousness due to a forceful displacement of the brain (e.g., by a blow to the head or sudden acceleration or deceleration).
Pathophysiology
Alerting or arousal is a function of the ARAS. Arousal to wakefulness is a prerequisite for awareness. This arousal system is anatomically represented by several structures in the rostral brainstem tegmentum, the diencephalon, and projections to the cerebral cortex.[8]Vincent SR. The ascending reticular activating system - from aminergic neurons to nitric oxide. J Chem Neuroanat. 2000 Feb;18(1-2):23-30.
http://www.ncbi.nlm.nih.gov/pubmed/10708916?tool=bestpractice.com
Principal among these are acetyl choline-producing neurons in the rostral brainstem. These project rostrally in 2 major pathways that also contribute to cortical arousal:[8]Vincent SR. The ascending reticular activating system - from aminergic neurons to nitric oxide. J Chem Neuroanat. 2000 Feb;18(1-2):23-30.
http://www.ncbi.nlm.nih.gov/pubmed/10708916?tool=bestpractice.com
A dorsal pathway that synapses with the midline and nonspecific thalamic nuclei, which then send a glutaminergic projection to large areas of the cerebral cortex
A ventral pathway from the rostral brainstem tegmentum that reaches the basal forebrain, especially the posterior hypothalamus, where axon terminals act on neurons that synthesize histamine, hypocretin, or orexin.
The ARAS is a complex system with some redundancy of pathways that are involved in arousal and maintenance of wakefulness. This may explain the recovery of the arousal system after initial coma, almost always within 3 weeks from coma onset in most patients. As a corollary, disorders cause impaired consciousness by impairing the function of a significant component of the ARAS.
Epidemiology
Although transient episodes of unconsciousness (e.g., faint, seizure) are common and account for about 5% of emergency room visits, in-hospital consultations for coma constitute only 0.02% of admissions in England.[9]Department of Health. Hospital Episode Statistics (England). 2002-2003 [internet publication].
http://www.hscic.gov.uk/hes
Adult men and women are almost equally affected. The mean age is 57 years, although >35% of patients with coma are >75 years of age.[9]Department of Health. Hospital Episode Statistics (England). 2002-2003 [internet publication].
http://www.hscic.gov.uk/hes
Prevention and management
Initial management steps include airway, breathing, and circulatory (ABC) support. In the unresponsive patient, airway protection is paramount.[10]Matthes G, Bernhard M, Kanz KG, et al. Emergency anesthesia, airway management and ventilation in major trauma. Background and key messages of the interdisciplinary S3 guidelines for major trauma patients [in German]. Unfallchirurg. 2012 Mar;115(3):251-64.
http://www.ncbi.nlm.nih.gov/pubmed/22406918?tool=bestpractice.com
Clinical assessment tools for patients with impaired consciousness, include the Glasgow Coma Scale and the Full Outline of UnResponsiveness (FOUR) scoring system; the latter has advantages in intubated patients.[11]Bruno MA, Ledoux D, Lambermont B, et al. Comparison of the Full Outline of UnResponsiveness and Glasgow Liege Scale/Glasgow Coma Scale in an intensive care unit population. Neurocrit Care. 2011 Dec;15(3):447-53.
http://www.ncbi.nlm.nih.gov/pubmed/21526394?tool=bestpractice.com
Guidelines inform the prevention and management of ischemic stroke, subarachnoid hemorrhage, intracerebral hemorrhage, and trauma.[12]Meschia JF, Bushnell C, Boden-Albala B, et al; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; Council on Hypertension. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014 Dec;45(12):3754-832.
http://stroke.ahajournals.org/content/45/12/3754.long
http://www.ncbi.nlm.nih.gov/pubmed/25355838?tool=bestpractice.com
[13]Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000375
http://www.ncbi.nlm.nih.gov/pubmed/34024117?tool=bestpractice.com
[14]Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-361.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000407
http://www.ncbi.nlm.nih.gov/pubmed/35579034?tool=bestpractice.com
[15]Hoh BL, Ko NU, Amin-Hanjani S, et al. 2023 guideline for the management of patients with aneurysmal subarachnoid hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2023 Jul;54(7):e314-70.
https://www.doi.org/10.1161/STR.0000000000000436
http://www.ncbi.nlm.nih.gov/pubmed/37212182?tool=bestpractice.com
[16]Centers for Disease Control and Prevention. Traumatic brain injury & concussion: prevention. May 2021 [internet publication].
https://www.cdc.gov/traumaticbraininjury/prevention.html
[17]National Institute for Health and Care Excellence. Head injury: assessment and early management. Sep 2023 [internet publication].
https://www.nice.org.uk/guidance/ng232
[18]Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury 4th edition. September 2016 [internet publication].
https://braintrauma.org/coma/guidelines/guidelines-for-the-management-of-severe-tbi-4th-ed
[19]Pandor A, Harnan S, Goodacre S, et al. Diagnostic accuracy of clinical characteristics for identifying CT abnormality after minor brain injury: a systematic review and meta-analysis. J Neurotrauma. 2012 Mar 20;29(5):707-18.
http://www.ncbi.nlm.nih.gov/pubmed/21806474?tool=bestpractice.com
[20]Coffeng SM, Foks KA, van den Brand CL, et al. Evaluation of clinical characteristics and CT decision rules in elderly patients with minor head injury: a prospective multicenter cohort study. J Clin Med. 2023 Jan 27;12(3).
https://www.mdpi.com/2077-0383/12/3/982
http://www.ncbi.nlm.nih.gov/pubmed/36769631?tool=bestpractice.com
[21]Kim YJ. A systematic review of factors contributing to outcomes in patients with traumatic brain injury. J Clin Nurs. 2011 Jun;20(11-12):1518-32.
http://www.ncbi.nlm.nih.gov/pubmed/21453293?tool=bestpractice.com
The use of pharmacological and electrical stimulation in cases of vegetative (UWS) and minimally conscious states remains controversial.[22]Oliveira L, Fregni F. Pharmacological and electrical stimulation in chronic disorders of consciousness: new insights and future directions. Brain Inj. 2011;25(4):315-27.
http://www.ncbi.nlm.nih.gov/pubmed/21314279?tool=bestpractice.com

Log in or subscribe to access all of BMJ Best Practice