Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- evidence or history of trauma
- focal neurologic deficit
- headache
- signs of elevated intracranial pressure (ICP)
- abnormal pupillary reflexes
Outros fatores diagnósticos
- loss of consciousness/decreased alertness
- cognition changes
- dysphasia
- seizure
- loss of bowel and bladder continence
- localized weakness
- sensory changes
- otorrhea
- rhinorrhea
Fatores de risco
- recent trauma
- coagulopathy and anticoagulant use
- advanced age (>65 years)
- excessive alcohol use
- intracranial hypotension (e.g., secondary to cerebral shunt or cerebrospinal fluid [CSF] leak)
Investigações diagnósticas
Primeiras investigações a serem solicitadas
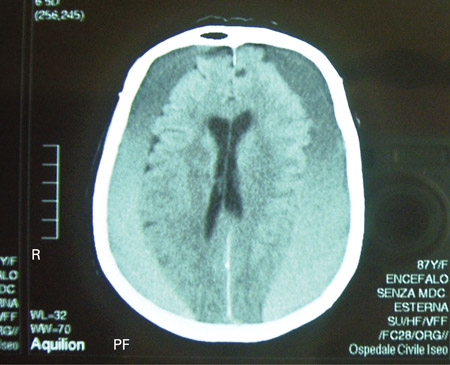
- noncontrast CT scan
Investigações a serem consideradas
- MRI scan
Algoritmo de tratamento
acute hematoma
chronic hematoma
Colaboradores
Autores
Christopher P. Robinson, DO, MS
Associate Professor of Neurology and Neurosurgery
Division of Neurocritical Care
Vice Chair of Clinical Operations
Neurology Clerkship Director
University of Florida College of Medicine
Florida
FL
Declarações
CPR has received compensation for serving as an expert witness.
Agradecimentos
Dr Christopher P. Robinson would like to gratefully acknowledge Dr Andrew W. Grande, Dr Stephen J. Haines, Dr Praveen R. Baimeedi, Dr Jason S. Hauptma, and Dr Neil A. Martin, previous contributors to this topic.
Declarações
AWG, SJH, PRB, JSH, and NAM declare that they have no competing interests.
Revisores
Nathan J. Ranalli, MD
Resident
Department of Neurosurgery
University of Pennsylvania School of Medicine
Philadelphia
PA
Declarações
NJR declares that he has no competing interests.
Marek Ma, MD
Instructor
Emergency Medicine
Department of Emergency Medicine Administrative Offices
University of Pennsylvania
Philadelphia
PA
Declarações
MM declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Expert Panel on Neurological Imaging; Shih RY, Burns J, Ajam AA, et al. ACR Appropriateness Criteria® head trauma: 2021 update. J Am Coll Radiol. 2021 May;18(5S):S13-36.Texto completo Resumo
American College of Surgeons. Best practice guidelines: the management of traumatic brain injury. 2024 [internet publication].Texto completo
Carney N, Totten AM, O'Reilly C, et al. Guidelines for the management of severe traumatic brain injury, Fourth Edition. Neurosurgery. 2017 Jan 1;80(1):6-15.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Epidural hematoma
- Intracerebral hematoma
- Diffuse axonal injury
Mais Diagnósticos diferenciaisDiretrizes
- Best practice guidelines in management of traumatic brain Injury
- Best practice guidelines in management of traumatic brain injury
Mais DiretrizesCalculadoras
Glasgow Coma Scale
Canadian CT Head Rule
Mais CalculadorasConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal