Summary
Definition
History and exam
Key diagnostic factors
- history of gastrointestinal (GI) surgery
- mental slowing, confusion, impaired concentration, and apathy
- oculomotor signs
- history of alcohol-use disorder
- pre-existing conditions that predispose to malnutrition: for example, HIV/AIDS, cancer, anorexia/bulimia, prolonged vomiting, or diarrhea
- classic triad: mental status changes, ophthalmoplegia, and gait dysfunction
Other diagnostic factors
- mild irritability
- acute psychosis
- coma
- miosis, anisocoria, light/near dissociation
- papilledema, retinal hemorrhages
- tachycardia or hypotension
- hypothermia or hyperthermia
- hearing loss, epileptic seizures, and spastic paraparesis
- ataxia
Risk factors
- alcohol-use disorder
- HIV infection and AIDS
- cancer and treatment with chemotherapeutic agents
- malnutrition
- history of gastrointestinal (GI) surgery
- genetic variants associated with altered thiamine metabolism and transport
- bone marrow transplantation
- male sex
Diagnostic tests
1st tests to order
- therapeutic trial of parenteral thiamine
- serum thiamine
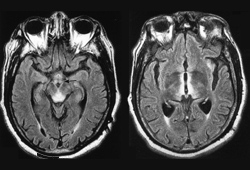
- MRI of brain
- blood glucose
- CBC
- serum electrolytes
- renal function
- LFTs
- toxicology screen
- serum ammonia
- blood alcohol level
Tests to consider
- lumbar puncture
Treatment algorithm
suspected Wernicke encephalopathy
high risk for thiamine deficiency
Contributors
Authors
Gregory S. Day, MD, MSc, MSCI, FAAN, FANA, FANA
Associate Professor of Neurology
Division Director, Behavioural Neurology
Mayo Clinic in Florida
Jacksonville
FL
Disclosures
GSD declares no competing interests directly relevant to this work. His research is supported by the National Institute of Health (U01AG057195, U01NS120901, U19AG032438). He serves as a consultant for Parabon NanoLabs, Inc. and as a topic editor (Dementia) for DynaMed (EBSCO). He is the co-project principal investigator for a clinical trial in anti-NMDAR encephalitis, which receives support from the National Institute of Neurological Disorders and Stroke (U01NS120901) and Amgen Pharmaceuticals, and a consultant for Arialys Therapeutics. He has developed and edited educational materials for Continuing Education, Inc. and Ionis Pharmaceuticals. GDS owns stock in ANI Pharmaceuticals. His institution has received support from Eli Lilly and Company for development and participation in an educational event promoting early diagnosis of symptomatic Alzheimer disease, and in-kind contributions of radiotracer precursors for tau-PET neuroimaging in studies of memory and aging (via Avid Radiopharmaceuticals, a wholly owned subsidiary of Eli Lilly and Company).
Acknowledgements
Dr Gregory S. Day would like to gratefully acknowledge Dr Abhay Moghekar, a previous contributor to this topic. AM is a medical advisory board member of the Hydrocephalus Association and was reimbursed for travel and airfare. AM was a consultant to Quest Diagnostics and Orbees Incorporation for market research, receiving payment for consulting. AM undertook research for Fujirebio Diagnostics and received a research grant to his lab at Johns Hopkins University.
Peer reviewers
Adrian Priesol, MD, FRCPC
Instructor
Massachusetts Eye and Ear Infirmary
Harvard Medical School
Boston
MA
Disclosures
AP declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Galvin R, Bråthen G, Ivashynka A, et al. Guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010 Dec;17(12):1408-18.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Alcohol intoxication
- Alcohol withdrawal
- Viral encephalitis
More DifferentialsGuidelines
- Guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer