Antiparasitic monotherapy recommended as treatment option for select cases of cystic echinococcosis
The World Health Organization (WHO) has published a new evidence-based guideline on the management options available for the treatment of cystic echinococcosis. The purpose of the guideline is to provide guidance on the choice of treatment so that patients can be offered appropriate, affordable, and equitable treatment in the context of available infrastructure and expertise to ensure safety and avoid unnecessary invasive interventions.
The WHO recommends treatment according to the stage and size of cysts. Treatment with albendazole (an antiparasitic agent) monotherapy is suggested for stage CE1, CE2, CE3a, and CE3b uncomplicated hepatic cysts that are less than 5 cm in size. For larger uncomplicated hepatic cysts, percutaneous, or surgical treatment is recommended depending on the cyst type, size, and response to initial treatment. Percutaneous and surgical treatments are often combined with albendazole. Praziquantel, given in combination with albendazole, is recommended after these procedures when cyst spillage is suspected or confirmed. Due to a lack of available data, these recommendations are based on very low-certainty evidence or expert consensus.
Inactive cysts (types CE4 and CE5) are typically treated with a “watch and wait” approach. Complicated hepatic cysts and pulmonary cysts are usually managed with surgery. However, a 6-month course of albendazole monotherapy may be considered in patients with small pulmonary cysts. However, it is uncertain whether albendazole alone can effectively treat these cysts.
Cystic echinococcosis represents a substantial disease burden in rural and pastoral communities in lower- and upper-middle-income countries. It is considered a significant problem in South America, North Africa, Eastern and Mediterranean Europe, the Russian Federation, the Middle East, Central Asia, and China
Resumo
Definição
História e exame físico
Principais fatores diagnósticos
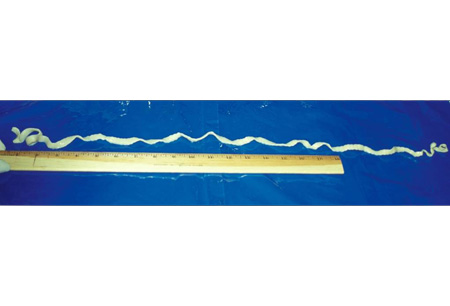
- worm segments in stool
- increased intracranial pressure
- seizures
- hepatomegaly
- cough
- hemoptysis
- chest pain
- allergy manifestations
- signs of anemia
Outros fatores diagnósticos
- asymptomatic
- vague intestinal symptoms
- sleep disturbance
- headaches
- rash
- subcutaneous nodules
- signs of sepsis
- right upper quadrant/epigastric pain
- dyspnea
- heart palpitations
- visual disturbances
Fatores de risco
- living on farms
- poor hygiene
- eating or handling undercooked meat
- eating or handling undercooked fish or crustaceans
- ingestion of contaminated water
- dog owners
- outdoor pursuits
- age <12 years
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- stool exam
- complete blood count
- enzyme-linked immunoelectrotransfer blot (EITB)
- echinococcus enzyme-linked immunosorbent assay (ELISA) and Western blot serology
- abdominal/thoracic ultrasound
- MRI of chest/abdomen
- echocardiogram
- CT of brain
- MRI of brain/spine
Investigações a serem consideradas
- screening for tuberculosis and strongyloidiasis
Algoritmo de tratamento
central nervous system disease: with elevated intracranial pressure
intestinal disease
central nervous system disease: without elevated intracranial pressure
hepatic or thoracic disease
Colaboradores
Autores
Jose A. Serpa, MD, MS, PhD
Professor of Medicine
Division of Infectious Diseases, Department of Medicine
University of Texas at Tyler
Tyler
TX
Declarações
JAS declares that he has no competing interests.
Agradecimentos
Dr Jose A. Serpa would like to gratefully acknowledge Dr Andrew Chou, Dr Christina Coyle, and Dr Maheen Saeed, previous contributors to this topic.
Declarações
AC and MS declare that they have no competing interests. CC is an author of several references cited in this topic.
Revisores
William A. Petri, Jr, MD, PhD, FACP
Chief and Professor of Medicine
Division of Infectious Diseases and International Health
University of Virginia Health System
Charlottesville
VA
Declarações
WAP declares that he has no competing interests.
Linda Kalilani, MBBS, MPhil, PhD
Epidemiologist
College of Medicine
University of Malawi
Zomba
Malawi
Declarações
LK declares that she has no competing interests.
Paul Roberts, MD
Assistant Professor
Family Medicine
Mayo Clinic
Jacksonville
FL
Disclosures
PR declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
World Health Organization. WHO guidelines for the treatment of patients with cystic echinococcosis. Jun 2025 [internet publication].Full text
White AC Jr, Coyle CM, Rajshekhar V, et al. Diagnosis and treatment of neurocysticercosis: 2017 clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2018 Apr 3;66(8):e49-75.Full text Abstract
World Health Organization. WHO guidelines on management of Taenia solium neurocysticercosis. Sep 2021 [internet publication].Full text
Del Brutto OH, Nash TE, White AC Jr, et al. Revised diagnostic criteria for neurocysticercosis. J Neurol Sci. 2017 Jan 15;372:202-10.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Central nervous system tuberculoma
- Amebic abscess
- Migraine
More DifferentialsGuidelines
- CDC Yellow Book: health information for international travel - post-travel parasitic disease including evaluation of eosinophilia
- WHO guidelines for the treatment of patients with cystic echinococcosis
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer