Summary
Definition
History and exam
Key diagnostic factors
- age 40-65 years
- female sex
- family history of PBC
Other diagnostic factors
- personal history of autoimmune disease
- family history of autoimmune disease
- history of hypercholesterolemia
- itch
- fatigue
- dry eyes and dry mouth
- abdominal discomfort
- sleep disturbance
- hepatomegaly
- xanthelasmata
- postural dizziness/blackouts
- memory and concentration problems
- jaundice
- ascites
- splenomegaly
- skin pigmentation
Risk factors
- female sex
- age between 40 and 65 years
- family history of PBC
- family history of autoimmune disease
- smoking
- urinary tract infection
Diagnostic tests
1st tests to order
- alkaline phosphatase (ALP)
- gamma-glutamyl transferase (GTT)
- bilirubin
- alanine aminotransferase (ALT)
- serum albumin
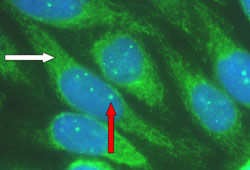
- antimitochondrial antibody (AMA) immunofluorescence
- antinuclear antibody (ANA) immunofluorescence
- antipyruvate dehydrogenase complex-E2 ELISA
- anti-M2 ELISA
- antiglycoprotein-210 ELISA
- anti-Sp100 ELISA
- abdominal ultrasound scan
- magnetic resonance cholangiopancreatography (MRCP)
- transient elastography
Tests to consider
- serum immunoglobulin
- liver biopsy
Treatment algorithm
early-stage disease
developing end-stage liver disease or refractory pruritus
Contributors
Authors
David Bernstein, MD
Professor of Medicine
NYU Grossman School of Medicine
Director, Gastroenterology and Hepatology
Ambulatory Network-Long Island
NYU Langone Health
New York
NY
Disclosures
DB is a consultant for Ipsen. DB is on the speakers bureau for Ipsen and Intercept.
Acknowledgements
Dr David Bernstein would like to gratefully acknowledge Dr David E. J. Jones, the previous contributor to this topic. DEJJ has received speaker honoraria from Falk, Intercept, and Abbott, grant funding from Intercept and Pfizer, and has undertaken consultancy work for Falk, GSK, Intercept, and Novartis. DEJJ is an author of a number of articles referenced in this topic.
Peer reviewers
James Neuberger, BM, BCh
Consultant Physician
Liver Unit
Queen Elizabeth Hospital
Birmingham
UK
Disclosures
JN declares that he has no competing interests.
Ian R. Mackay, AM, MD, FAA, FRACP, FRCPA, FRCP
Department of Biochemistry and Molecular Biology
Monash University
Clayton
Victoria
Australia
Disclosures
IRM declares that he has no competing interests.
Alia S. Dadabhai, MD
Assistant Professor
Gastroenterology and Hepatology Division
Johns Hopkins University
Baltimore
ML
Disclosures
AD declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Lindor KD, Bowlus CL, Boyer J, et al. Primary biliary cholangitis: 2018 practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2019 Jan;69(1):394-419.Full text Abstract
European Association for the Study of the Liver. EASL clinical practice guidelines: the diagnosis and management of patients with primary biliary cholangitis. J Hepatol. 2017 Jul;67(1):145-72. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Obstructive bile duct lesion
- Small-duct primary sclerosing cholangitis
- Drug-induced cholestasis
More DifferentialsGuidelines
- AASLD practice guideline on imaging-based non-invasive liver disease assessments of hepatic fibrosis and steatosis
- EASL clinical practice guidelines on non-invasive tests for evaluation of liver disease severity and prognosis - 2021 update
More GuidelinesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal