Summary
Definition
History and exam
Key diagnostic factors
- history of opioid use disorder and dependence
- miosis
- bradypnea
- altered mental status
- dramatic response to naloxone
Other diagnostic factors
- fresh needle marks
- drug paraphernalia nearby
- decreased gastrointestinal motility
- old track marks on arms and legs
- pulmonary rales
- frothy pink sputum
- seizures
- dysrhythmias
Risk factors
- opioid use disorder and dependence
- recent abstinence in chronic users
- chronic pain
Diagnostic tests
1st tests to order
- therapeutic trial of naloxone
- Electrocardiogram (ECG)
Tests to consider
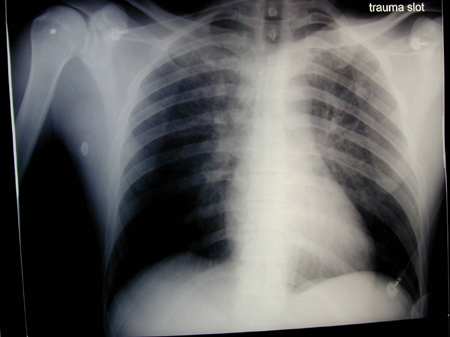
- chest x-ray
- abdominal x-ray
- abdominal CT scan
- opioid urine screen
- gas chromatography/ mass spectrometry
Treatment algorithm
patients with signs of opioid overdose or toxicity: in cardiac arrest
patients with signs of opioid overdose or toxicity: not in cardiac arrest
Contributors
Authors
Ruben Thanacoody, MD, FRCP
Consultant Physician and Clinical Toxicologist
Director, National Poisons Information Service (Newcastle)
Newcastle-upon-Tyne
UK
Disclosures
RT declares that he has no competing interests.
Acknowledgements
Dr Ruben Thanacoody would like to gratefully acknowledge Dr Dean Olsen, a previous contributor to this topic.
Disclosures
DO declares that he has no competing interests.
Peer reviewers
William Winter, MD
Staff
Gynecologic Oncologist
Northwest Cancer Specialists
Rose Quarter Cancer Center
Portland
OR
Disclosures
WW declares that he has no competing interests.
Anne-Maree Kelley, MD, MClinEd, FACEM
Director
Joseph Epstein Centre for Emergency Medicine Research
Western Health Sunshine Hospital
St Albans
Australia
Disclosures
AMK has received grant funding for research into intranasal delivery of naloxone in heroin overdose.
Andrew Stolbach, MD
Assistant Professor
Johns Hopkins University
Baltimore
MD
Disclosures
AS declares that he has no competing interests.
References
Key articles
Dowell D, Ragan KR, Jones CM, et al. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. 2022 Nov 4;71(3):1-95.Full text Abstract
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Evidence-based strategies for preventing opioid overdose: what’s working in the United States. 22 October 2020 [internet publication].Full text
Dezfulian C, Orkin AM, Maron BA, et al. Opioid-associated out-of-hospital cardiac arrest: distinctive clinical features and implications for health care and public responses: a scientific statement from the American Heart Association. Circulation. 2021 Apr 20;143(16):e836-70.Full text Abstract
Resuscitation Council UK. 2021 resuscitation guidelines. 2021 [internet publication].Full text
Williams K, Lang ES, Panchal AR, et al. Evidence-based guidelines for EMS administration of naloxone. Prehosp Emerg Care. 2019 Nov-Dec;23(6):749-63.Full text Abstract
Lavonas EJ, Akpunonu PD, Arens AM, et al. 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023 Oct 17;148(16):e149-84.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Gammahydroxybutyrate (GHB)/gammabutyrolactone (GBL) overdose
- Clonidine/imidazolines overdose
- Antipsychotic overdose
More DifferentialsGuidelines
- 2023 American Heart Association focused update on the management of patients with cardiac arrest or life-threatening toxicity due to poisoning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care
- Clinical practice guideline for prescribing opioids for pain
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer